More Information
Submitted: December 05, 2024 | Approved: February 03, 2025 | Published: February 04, 2025
How to cite this article: Alieva MU, Nadzhmutdinova NS, Abdukayumov AA, Inoyatova FI, Musaev MM, Abdullaeva MI. Analysis of Acoustic Parameters of Voice Jitter and Shimmer in Children with Dysphonia after Laryngeal Surgery. Arch Case Rep. 2025; 9(2): 044-050. Available from:
https://dx.doi.org/10.29328/journal.acr.1001126
DOI: 10.29328/journal.acr.1001126
Copyright license: © 2025 Alieva MU, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Rehabilitation; Vocal apparatus; Voice quality; Larynx; Acoustic analysis
Analysis of Acoustic Parameters of Voice Jitter and Shimmer in Children with Dysphonia after Laryngeal Surgery
Munira Ulugbekovna Alieva1*, Nozima Shamsutdinovna Nadzhmutdinova1, Abdumannap Abdumazhidovich Abdukayumov1, Flora Ilyasovna Inoyatova1, Muhammadjon Makhmudovich Musaev2 and Malika Ilkhamovna Abdullaeva2
1The Republican Specialized Scientific and Practical Medical Center of Pediatrics (RSSPMCP), Tashkent, Republic of Uzbekistan
2Tashkent University of Information Technologies named after Muhammad al-Khwarizmi, Tashkent, Republic of Uzbekistan
*Address for Correspondence: Munira Ulugbekovna Alieva, The Republican Specialized Scientific and Practical Medical Center of Pediatrics (RSSPMCP), Tashkent, Republic of Uzbekistan, Email: [email protected]
The article conducted a study of computer acoustic analysis of Jitter and Shimmer voice parameters in children with dysphonia after laryngeal surgery. The study found that children with dysphonia had significantly lower preoperative Jitter and Shimmer scores (574359, 587, and 2.3) compared to healthy children (1316743.376 and 4.84). At 1 month after surgery, affected children showed a decrease in Jitter and Shimmer indices compared with these acoustic indices before surgery. However, at 2 months, there was a significant increase in Jitter and Shimmer scores, and at 3 months, Jitter and Shimmer scores were comparable to Jitter and Shimmer scores in healthy children without dysphonia. The results of the study show that the method of analyzing the acoustic parameters of the voice Jitter and Shimmer allows a phoniatrist to objectively assess the occurrence of a voice disease in patients with dysphonia, and this method is the most accurate criterion for determining the pathologies of dysphonia and determining the treatment program for the disease.
The voice is an instrument of interpersonal communication, so the quality of the voice is of great importance for the social adaptation of the child in society. Dysphonia is a disorder of vocal function, which is expressed by weakness, hoarseness, and hoarseness of the voice of children in the form of hoarseness of varying degrees from acute laryngitis to severe lesions of respiratory papillomatosis and diseases of the larynx (vocal cord nodules, unilateral paresis of the vocal cords). With dysphonia, a change in the voice of children occurs in the form of hoarseness of varying degrees of severity from a dull voice to a complete absence of voice. Long-term dysphonia is a psychotraumatic factor, often leading to disruption of the child’s social adaptation [1]. With dysphonia, important functions of the larynx are disrupted, such as voice formation, breathing problems, and in some cases, swallowing disorders may develop. All this affects the quality of life and severe dysfunction of the larynx in children, they can have a negative effect on the child’s social adaptation and speech development. Modifying factors for dysphonia (factors leading to or provoking dysphonia) can be: operations directly on the larynx or manipulations to ensure emergency airway patency, which can lead to changes in the structure of the larynx and voice pathology [2]. When diagnosing the condition of the larynx, a subjective assessment of the voice is the Voice Handicap Index (VHI) questionnaire [3], and the most used, valid, and reliable questionnaire is the nine-item International Voice Handicap Index (VHI-9i) questionnaire - the clinically established version the original VHI, which quantifies patient-reported voice impairment [4]. The initial examination of a patient with dysphonia is based on a thorough history taking, analysis of the patient’s complaints, and clinical examination. Traditionally, invasive methods such as flexible and rigid fiberscopic laryngoscopy (examination using a fiber-optic instrument), video stroboscopy (strobe lighting of the larynx), and electromyography (indirect observation of the functional state of the larynx) are used to diagnose dysphonia. Improvement of standard endoscopy and the introduction of modern technologies into otorhinolaryngology, which allow for a better examination of all parts of the larynx, make it possible to assess the anatomical features of the functioning of the larynx, but assessing voice quality is quite difficult.
Currently, the diagnosis and effective treatment of dysphonia is ensured by the introduction into the practice of a phoniatrist of modern innovative methods for assessing the state of the vocal function of the larynx. When diagnosing dysphonia and assessing the voice quality of patients with dysphonia, a method of analyzing the parameters of the acoustic signal is used - auditory-perceptual voice analysis [5,6]. The method of computer spectral acoustic analysis of voice (AAG) is a non-invasive method for diagnosing dysphonia, which is based on subjective and objective data from the patient’s voice [7,8]. Acoustic analysis is an objective, non-invasive screening method to identify laryngeal pathology and assess voice quality in patients with voice disorders such as laryngitis, laryngospasm, laryngeal tumors, spasmodic dysphonia, vocal cord paralysis, etc. [9,10]. In paper [11], when conducting a computer spectral analysis of the voice, 5 indicators of acoustic parameters of the voice were measured: Energy of discrete signals, Entropy, Maximum signal value, Minimum signal value, Zero points number, and spectrograms of the acoustic parameters of the voices of children with dysphonia and healthy children were obtained.
Thus, modern diagnostics of the functioning of the larynx is very diverse and its assessment is one of the key factors in the effective treatment of dysphonia in children.
The human speech production system consists of a set of soft tissue components of the larynx. Since the vibrations of the vocal folds are not strictly periodic, there are always small fluctuations in it. Jitter and Shimmer are acoustic characteristics of vocal signals that are caused by irregular vibration of the vocal cords.
A study of the literature data [12,13] showed that Jitter and Shimmer can be used to diagnose voice disorders in dysphonia, and the analysis of these acoustic parameters of the voice can help in assessing the degree of voice instability and visually undetectable pathologies. There are several different ways to measure jitter and flicker. For example, when voice disorders are identified, they are measured as a percentage of the average period, with values above certain thresholds potentially associated with pathological voices. Jitter and flicker are most noticeable in long, sustained vowels.
A paper [14] shows, that in order to assess the functional state of the larynx, in an еpostoperative examination of 45 patients aged 18 to 70 years, a decrease in frequency instability (Jitter, %) was observed: before surgery - 1.18, after surgery on the 14th day - 0.09, and after 1 month - 0.025, and there was also a decrease in voice instability in amplitude (Shimmer,%): before surgery - 14.2, after surgery on 14th day – 6.08, and after 1 month – 3.95.
Analysis of the acoustic characteristics of the voice Jitter and Shimmer has the advantage of providing objective data for assessing voice disorders in patients with dysphonia and becoming an indispensable method for detecting voice diseases and voice disorders. However, to date, clear algorithms and criteria for assessing the voice quality of children with dysphonia using the acoustic method, which is often based on subjective assessments, have not been developed.
In the literature, there is no data on the study and analysis of the acoustic characteristics of the Jitter and Shimmer voices in children with dysphonia after laryngeal surgery.
The purpose of this work is to develop a methodology for measuring the acoustic parameters of the Jitter and Shimmer voice and to study and analyze the obtained acoustic parameters of Jitter and Shimmer to monitor the rehabilitation process of children with dysphonia after laryngeal surgery.
For the first time, in the department of congenital and industrial diseases of the ENT organs of the Republican Specialized Scientific and Practical Medical Center of Pediatrics, studies were conducted to study and analyze pre- and postoperative studies of the acoustic parameters of the voice of Jitter and Shimmer in sick children with dysphonia.
This study was approved by the institutional ethics committee of RSSPMCP. A medical examination of the patients was made after the informed consent of the parents and the examination included: a thorough collection of anamnesis (medical history) and analysis of complaints, preliminary listening and assessment of voice quality (speech), visualization of the larynx ENT organs using the endoscopic method and computer acoustic analysis of Jitter and Shimmer voice characteristics.
The age characteristics revealed that 61.3% (n = 57) of children were under the age of 6 years, which indicates that chronic pathology of the larynx develops precisely in the younger age category (Table 1).
| Table 1: Distribution of patients by gender and age. | ||||||
| Gender | Age | Total | ||||
| 4-6 years | 7-10 years | 11-17 years | absolutely | % | ||
| Boys | 38 | 10 | 6 | 54 | 58.1 | |
| Girls | 19 | 9 | 11 | 39 | 41.9 | |
| Total | absolutely | 57 | 19 | 17 | 93 | 100.0 |
| % | 61.3 | 20.4 | 18.3 | |||
All patients with dysphonia were assessed using the following methods:
Visualization of the larynx was done using endoscopic methods - fibrorhinolaryngoscopy with video recording (C-MAC, K. Storz, Ø-2.7 mm), telelaryngoscopy 700, direct microlaryngoscopy, MDCT (multidetector computed tomography) of the larynx in 3D mode with virtual laryngoscopy. Fibrorhinolaryngoscopy was performed with a flexible laryngoscope with the smallest distal end size (Ø-2.7 mm), with a camera at the distal end and video recording, without additional sedation and the use of local anesthetics. The study time was up to 5 minutes, no special preparation of patients was required, and the time of the last meal was at least 3 hours before the study. The study made it possible to conduct endoscopy in children under 6 years of age with good visualization of the lumen of the larynx and determination of pathological processes; it is also possible to conduct endoscopy in older children if it is difficult to study with rigid endoscopy due to emotional problems. Videotelaryngostroboscopy (VLS) at a viewing angle of 700 and 900 to the tissue surface in children over 7 years of age was performed. This method is a well-established procedure that analyzes the vibration of the vocal cords, but it has become a routine test for voice problems. VLS is critical to assessing the patient with dysphonia and their progress. The use of the VLS method increases diagnostic accuracy in 68.3% of cases of hoarseness. Direct microlaryngoscopy under general anesthesia using a microscope of the OPMI® Sensera™ Carl Zeiss system (Germany) with complemented endoscopes with a viewing angle of 00 and 300 was performed.
MDCT of the larynx in 3D mode with virtual laryngostracheoscopy (Sensation16, Siemens, Germany) was performed with a standard distance between the X-ray film and the radiation source of 100 cm, and studies in direct, lateral, and oblique projections were mandatory. The tomograph step was 2 mm, and the slice thickness was 2 mm. The data obtained were processed using a special program with the production of 3D images in virtual endoscopy mode.
Auditory-perceptual analysis was carried out using the N. Yanagihara scale (1967), which is a classic method for determining the degree of dysphonia. Voice quality was assessed on a scale from 0 to 5, and only one characteristic of the voice was examined - the sonority of the voice or the degree of hoarseness: 0 - normal voice; 1 – dull voice; 2 – mild degree of hoarseness; 3 – moderate degree of hoarseness; 4 – severe degree of hoarseness; 5 – aphonia.
Acoustic measurements of the fundamental tone frequency (FFT) of the vocal folds were determined with a laryngostroboscope mPulsar (K. Storz, Germany) when patients pronounced the drawn-out vowel “and” (at this time a video image of the larynx appears on the monitor screen). Time of maximum phonation (TMP), a method for determining the duration of a sound, was measured using a stopwatch, which recorded the time during which the patient pronounced the vowel sound /i/, the sound intensity of which should correspond to spoken speech. The VMF measurements were carried out three times and the average value of the result was recorded (the unit of measurement is seconds). The ТMF method was used to determine the degree of closure of the vocal cords during the duration of sound vibrations. According to work [15], shortening (decrease) of the VMF to 5 seconds in children 5–7 years old and up to 9 seconds in children 8–12 years old indicates insufficient closure of the vocal cords.
A special soundproof room was used to collect data and analyze the acoustic characteristics of the Jitter and Shimmer voices of children with dysphonia. The patients’ voice was recorded using a microphone equipped with a built-in noise level meter. The microphone at a distance of 30 cm from the child’s mouth was placed. The voices of children with dysphonia after surgery on the larynx and healthy children in the control group were recorded when they pronounced the vowel sound /i/. The optimal mode for voice recording was determined to be a noise level of no more than 40 dB. Audio signals of wav format with a sampling frequency of 22050 Hz and monotype on a computer were recorded using the computer program for recording audio data “Audacity”. The use of the Audacity program is due to the power of the program, which records and processes voice messages, including cleaning the recorded sound from noise and normalizing sound waves by height [16]. The results of audio recordings of the voices of children of patients before surgery on the larynx and after surgery after 1, 2, and 3 months of rehabilitation of patients were analyzed based on objective indicators of the acoustic parameters of the voices of patients Jitter and Shimmer.
The main criteria for the parameters of Jitter and Shimmer are effects, the level of turbulent noise, and the nonlinearity of the process of vibration of the vocal cords [17].
Jitter is defined as the change in frequency from cycle to cycle, and Shimmer refers to the change in amplitude of the sound wave [18]. Jitter is affected primarily by a lack of control of vocal cord vibration, and the voices of patients with pathology often have a higher percentage of Jitter.
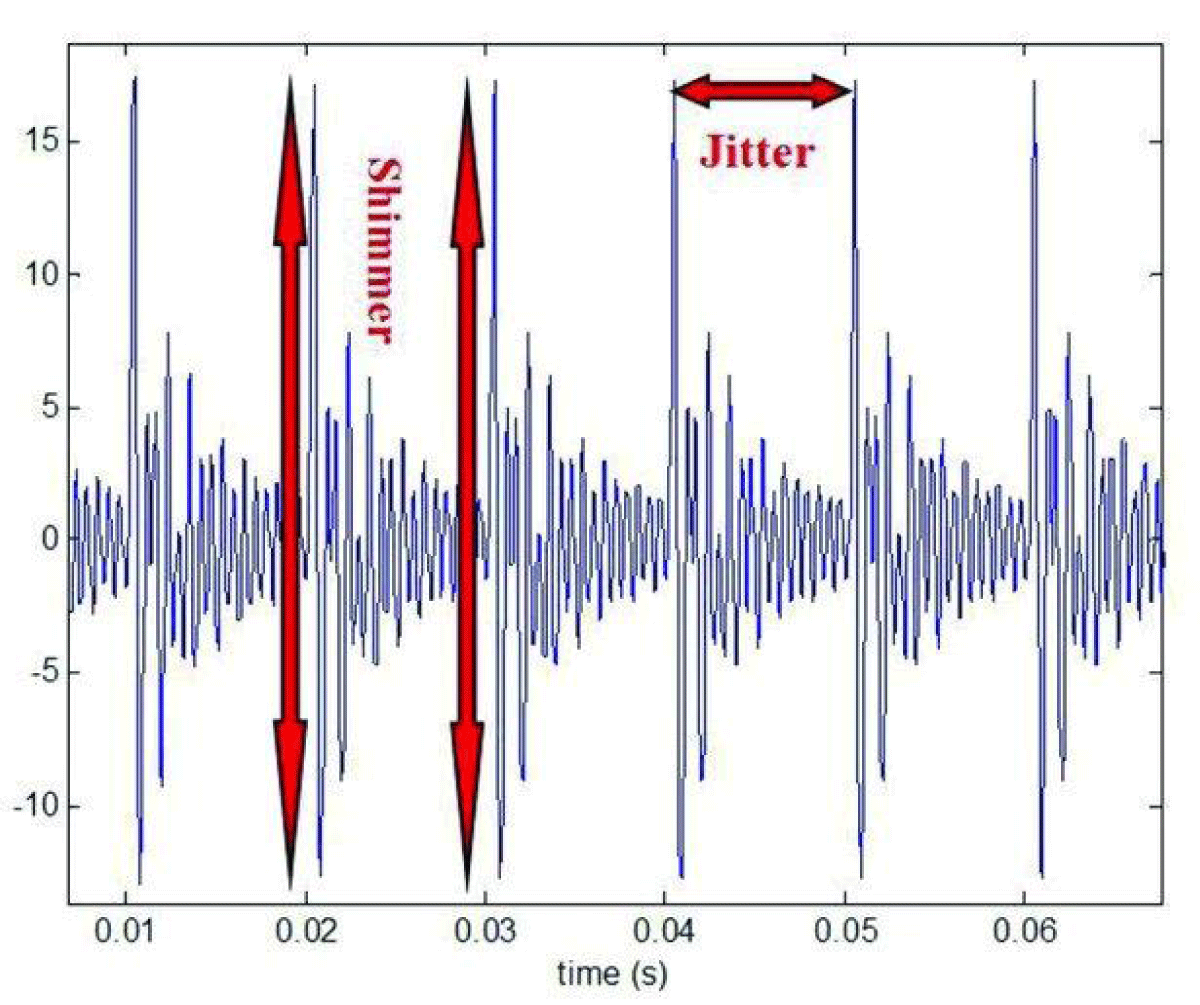
Jitter is the measure of the cycle-to-cycle variations of the fundamental glottal period and shimmer is the cycle-to-cycle variations of the fundamental glottal period amplitudes as depicted in Figure 1.
Figure 1: Measures of disturbances Jitter and Shimmer in a speech signal [6].
Jitter is commonly used to assess temporal instability in an acoustic speech signal, which characterizes changes in the time intervals between successive pitch periods due to physiological or psychological factors. Jitter may reflect some aspects of dysphonia, but its usefulness for the full assessment of dysphonia is limited. The Jitter score may be useful in the context of general acoustic analysis of the voice and may complement other methods for diagnosing dysphonia, such as visual assessment of dysphonia. However, Jitter cannot fully capture the diversity of symptoms and causes of dysphonia [7].
There are various methods for calculating and estimating the Jitter parameter for speech signals. Jitter is defined as the standard deviation of the time differences between successive pitch periods:
Where, P(i+1) and Pi are durations of the i-th and i+1-th main tonal periods, respectively; N is the total number of periods in the speech signal.
Jitter is mainly affected by the lack of vibration control of the vocal folds [9].
Jitter and Shimmer is a measure of pitch variability in an acoustic speech signal that evaluates changes in the amplitude of pitch periods. If Ai is the amplitude of the i-th period of the fundamental tone, Pi is the duration of the i-th period of the fundamental tone, then the local shimmer for the same segment can be mathematically represented by the following formula:
Where: A – average amplitude of the periods of the fundamental tone;
N is the total number of periods in the speech signal.
The Jitter value is mainly influenced by the lack of control of vocal fold vibration, while the Shimmer value is influenced by decreased glottal resistance and mass lesions of the vocal folds, which are associated with the presence of noise during aspirated emissions [19]. For stable phonation in children, the typical change in Jitter value is between 0.5% and 1.0%. Shimmer changes with decreased vocal impedance and volumetric lesions of the vocal cords, correlates with the presence of noise emissions and dyspnea, and is considered pathological voice for children with values of about 0.4% and 1% [20].
Visual examination revealed laryngeal pathologies in all sick children and diagnosed the following types of dysphonia: laryngeal membranes in 8 children (8.6%); the largest number were sick children with respiratory recurrent papillomatosis (RRP) - 58 children (62.3%), sick children with vocal cord nodules (VCN) - 18 children (19.3%), sick children with cicatricial changes in the larynx due to causes medical nature – 9 children (9.6%) (Table 2).
| Table 2: Characteristics of patients with dysphonia according to nosology. | ||
| Pathology | Quantity | Indicator, % |
| Laryngeal membranes | 8 | 8,6 |
| RRP | 58 | 62,3 |
| VCN | 18 | 19,3 |
| Scar changes in the larynx due to medical reasons | 9 | 9,6 |
Table 1 shows the average values of the voice parameters Jitter and Shimmer for children with dysphonia after laryngeal surgery.
When studying dysphonia using the auditory-perceptual analysis method, severe dysphonia was detected in 26.9% of patients, while aphonia developed in 13.9% of children (children after operations associated with RRP and surgical interventions for the elimination of laryngeal stenoses and congenital membranes). The average degree of development of dysphonia in children with RRP and vocal nodules identified with the largest number was 44.1% (Table 3).
| Table 3: Indicators of voice changes in benign laryngeal formations in children (N. Yanagihara, 1967). | |||||
| Dysphonia degree | Pathology of the larynx | Total, n/ % |
|||
| RRP, n = 8 |
VCN, n = 8 |
Cicatricial stenoses caused by laryngeal surgery, n = 9 | Laryngeal membranes, n = 8 | ||
| 0 - normal voice | - | - | - | 0 | |
| 1 – muffled voice | - | - | - | 0 | |
| 2 – mild hoarseness; | - | 10 | 2 | 2 | 14/15,0 |
| 3 – moderate hoarseness; | 29 | 8 | 3 | 1 | 41/44,1 |
| 4 – severe hoarseness; | 25 | - | - | 25/26,9 | |
| 5 – aphonia | 4 | - | 4 | 5 | 13/13,9 |
The criteria for RRP were more severe degrees of hoarseness from average to aphonia, which was constant, without periods of improvement, while the increase in the degree of hoarseness was accompanied by the appearance of shortness of breath and its intensification.
The criteria for VCN were mild to moderate dysphonia, of an unstable nature, which changed throughout the day, while the morning voice was always much better than the evening voice. Dysphonia was never accompanied by shortness of breath or dysphagia.
The criteria for vocal cord membranes were most often pronounced dysphonia; with membranes extended in-depth, they were accompanied by complete aphonia; with membranes in the form of a “crow’s foot”, hoarseness was grade 3-4.
Cicatricial stenoses caused by medical reasons led to dysphonia of 2-3-4 degrees, rarely to aphonia, since most often cicatricial changes were localized in the subglottic area, partially involving the lower surface of the vocal cords, while with the membranes of the larynx, the pathology was directly located in areas of voice formation, namely on the vocal cords.
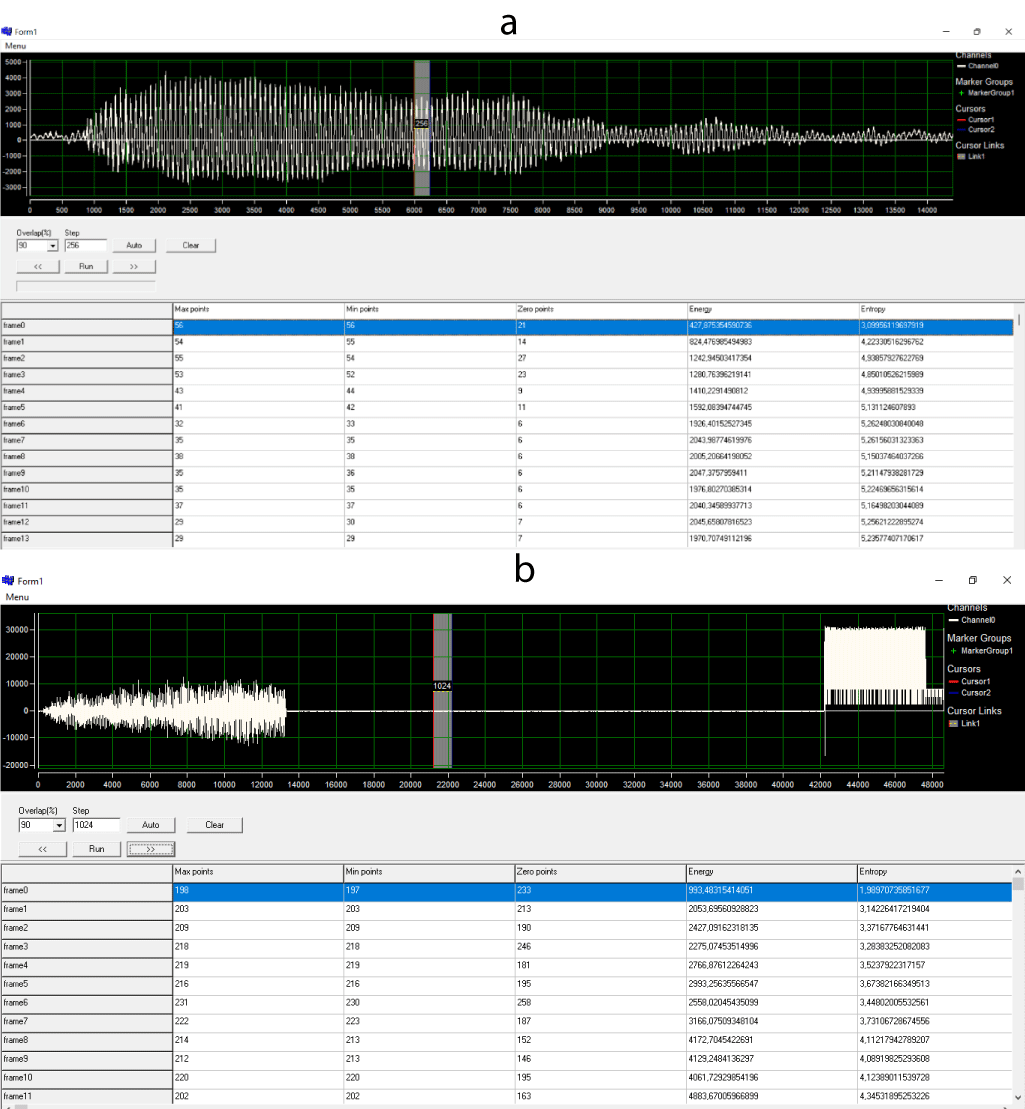
Figure 2 shows signalgrams of an audio recording of the voice of a healthy child (a) and a sick child with dysphonia after surgery on the larynx (b).
Figure 2: a) Signalogram of audio recordings of the voice of a healthy child. b) Signalogram of audio recordings of the voice of a sick child with dysphonia.
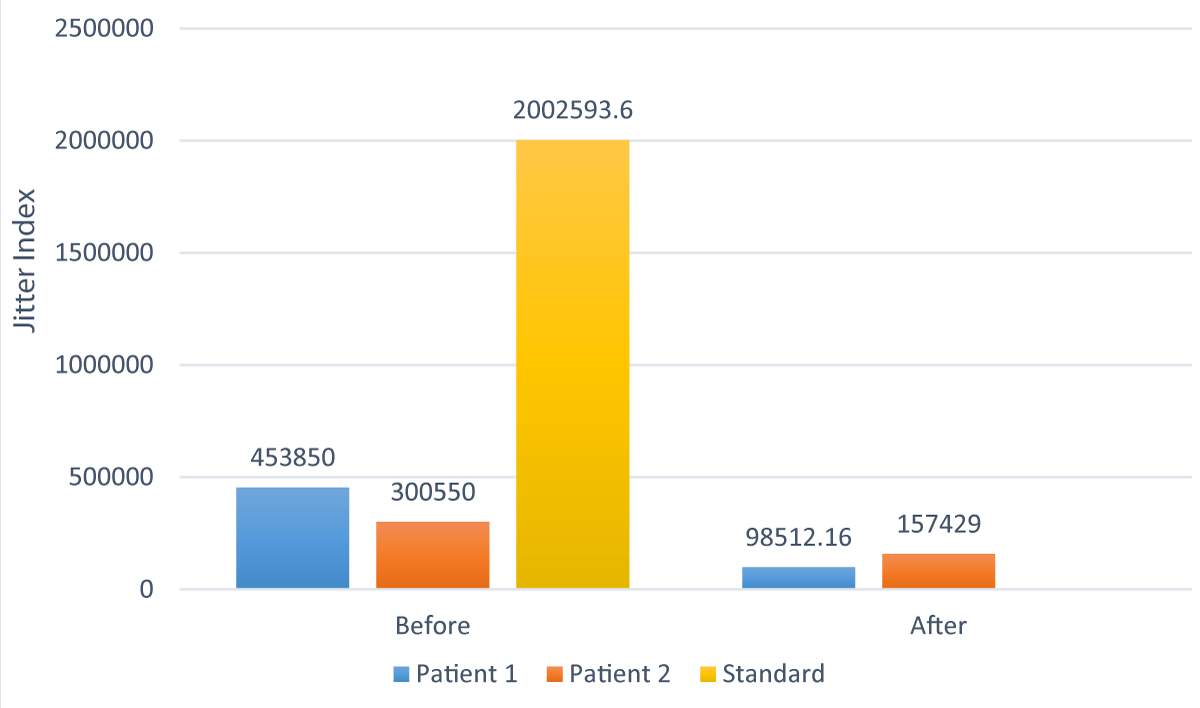
Table 4 shows the results of the Jitter and Shimmer acoustic voice parameters of a sample of three children with dysphonia 1 month and 2 months after laryngeal surgery.
| Table 4: The results of the Jitter and Shimmer acoustic voice parameters of a sample of three children with dysphonia 1 month and 2 months after laryngeal surgery. | |||||
| Acoustic indicator | Before surgery | After 1 month after surgery on the larynx |
Decrease in indicator after surgery, % | After 2 months after surgery |
Increase in indicator after surgery, % |
| Acoustic characteristics of the voice of a sick child (patient) No. 1 | |||||
| Jitter | 453 850. 26 | 98 512.16 | 21.71 | 723 788.31 | 159.5 |
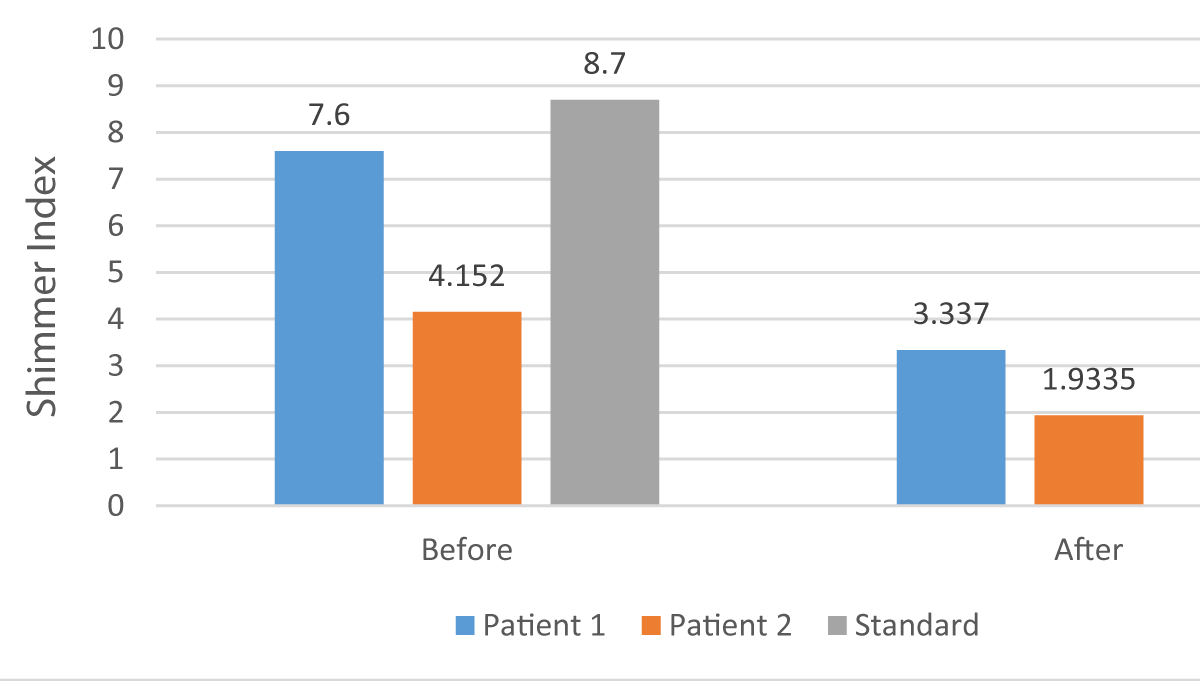
| Shimmer | 7.149 | 3.337 | 46.7 | 7.89 | 110.4 |
| Acoustic characteristics of the voice of a sick child (patient) No. 2 | |||||
| Jitter | 300 550 | 157 429 | 52,4 | 388 347 | 129.2 |
| Shimmer | 4.152 | 1.9335 | 46.6 | 4. 812 | 115.9 |
| Acoustic characteristics of the voice of a sick child (patient) No. 3 | |||||
| Jitter | 675 933 | 405 846 | 60.0 | 826 923 | 122,3 |
| Shimmer | 6.3 | 4.508 | 71.6 | 6.557 | 104.1 |
As can be seen from Table 4, in a sample of three patients 1 month after surgery on the larynx, there is a decrease in the acoustic parameters of the voice Jitter from 21.71% to 60.0% and Shimmer from 46.6% to 71.6% compared to these the same indicators before laryngeal surgery. However, 2 months after rehabilitation, an increase in the acoustic parameters of Jitter from 122.3% to 159.5% and Shimmer from 104.1 to 115.9% is observed compared to these indicators before the larynx surgery. The results obtained indicate the dynamics of the process of rehabilitation of sick children after laryngeal surgery.
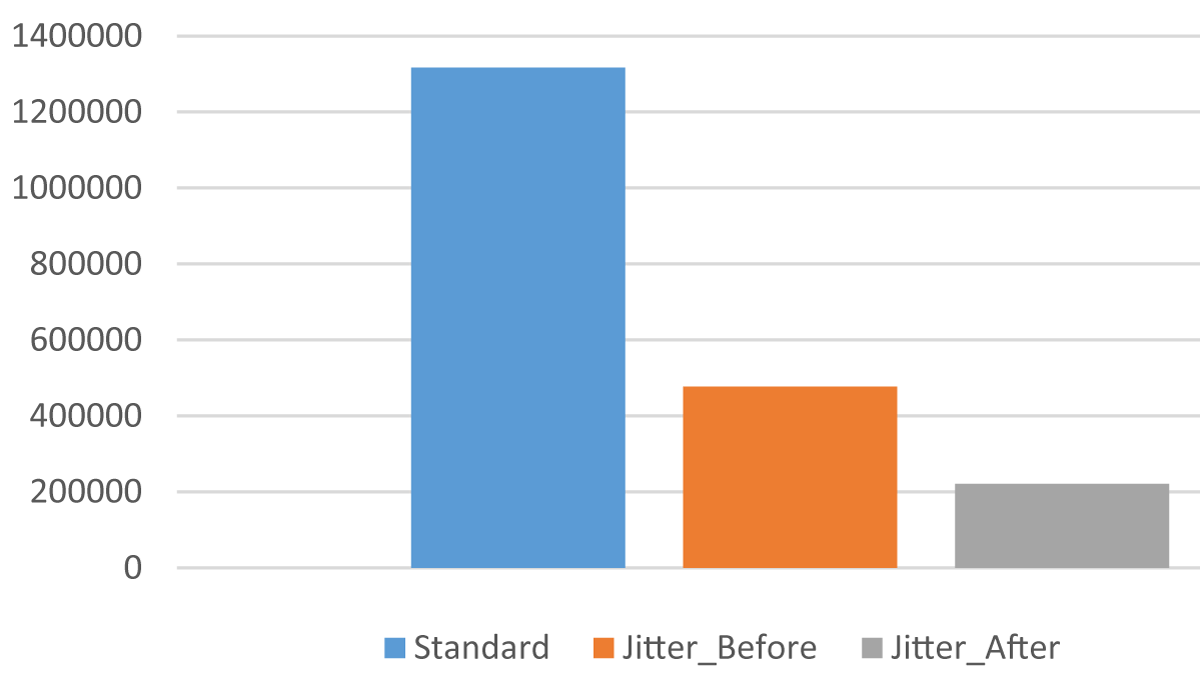
Figure 3 shows a comparison of the “i” sound based on the Jitter.
Figure 3: Comparison of the sound “i” based on the Jitter.
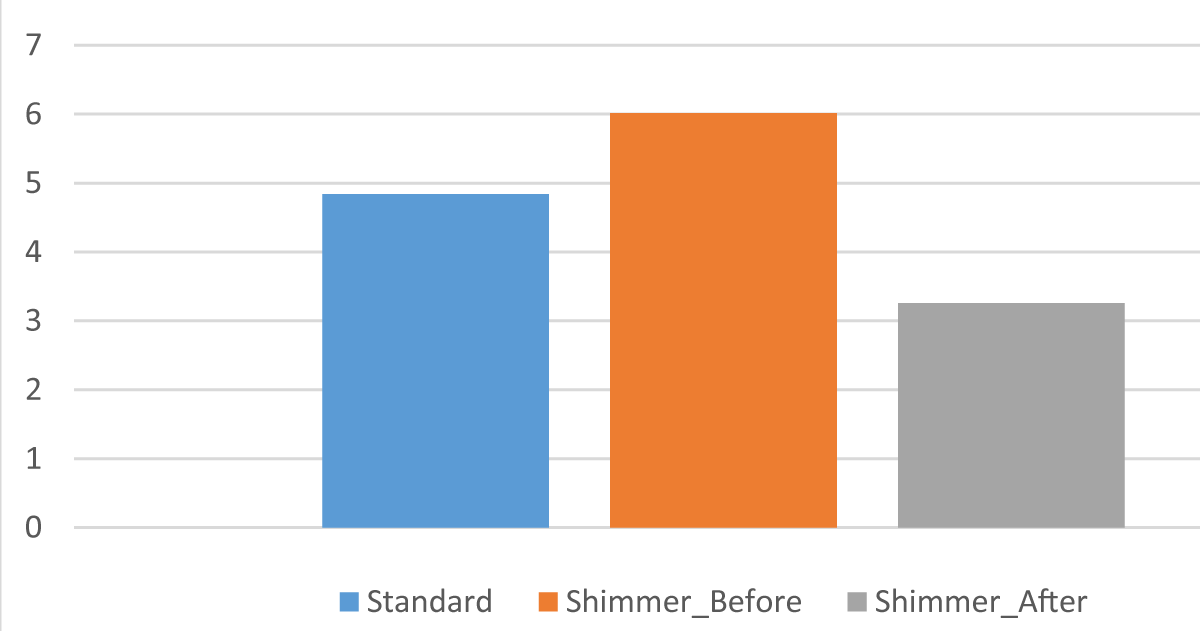
Figure 4 shows a comparison of the “i” sound based on the Shimmer.
Figure 4: Comparison of the sound “i” based on the Shimmer.
Figure 5 shows a comparison of average Jitter values.
Figure 5: Comparison of average Jitter values.
Figure 6 shows a comparison of average Shimmer values.
Figure 6: Comparison of average Shimmer values.
Table 5 shows the arithmetic mean values of the acoustic parameters of the voice Jitter and Shimmer of all 93 studied children with dysphonia after laryngeal surgery.
| Table 5: Average value of Jitter and Shimmer parameters in children with dysphonia after laryngeal surgery. | ||
| Jitter | Shimmer | |
| Patients with dysphonia before surgery | 574 359.587 | 2.3 |
| Patients with dysphonia after surgery 1 month later | 363 945.925 | 1.28 |
| Patients with dysphonia after surgery 2 months later | 925 233.732 | 3.14 |
| Patients with dysphonia after surgery 3 months later | 1 292 562.982 | 4.22 |
| Healthy children without dysphonia | 1 316 743.376 | 4.84 |
The research results showed (Table 5), that children with dysphonia before laryngeal surgery had significantly lower Jitter and Shimmer scores (574359.587 and 2.3) compared to healthy children (1316743.376 and 4.84). Moreover, 1 month after surgery, sick children showed a noticeable decrease in Jitter and Shimmer indices compared to these acoustic indices before surgery. However, at 2 months, there was a significant increase in Jitter and Shimmer scores, and at 3 months Jitter and Shimmer scores were comparable to Jitter and Shimmer scores in healthy children without dysphonia. The experimental data obtained confirm the complete rehabilitation and recovery of sick children with dysphonia after laryngeal surgery.
Analysis of the acoustic parameters Jitter and Shimmer in children with dysphonia after laryngeal surgery has advantages over other diagnostic methods in terms of non-invasiveness, low price, convenience, and objectivity.
The results of a study of the acoustic parameters of the Jitter and Shimmer voice in children with dysphonia showed that by measuring the acoustic parameters of the Jitter and Shimmer voice and comparing them with similar indicators in healthy children, it is possible to effectively monitor and control the dynamics of the progress of the rehabilitation of children after laryngeal surgery.
Thus, the method of analyzing the acoustic parameters of the voice Jitter and Shimmer provides an opportunity for a phoniatrist to objectively assess the course of the disease of the vocal apparatus of children with dysphonia, and this method has proven to be most useful for determining pathology and clarifying a therapeutic rehabilitation program.
The authors wish to express their gratitude to all the staff of the Department of Congenital and Industrial Diseases of the ENT Organs of the Republican Specialized Scientific and Practical Medical Center of Pediatrics Tashkent, Uzbekistan.
- Radzig EY, Bulynko YE, Orlova OS. Voice disorders in children at different stages of speech development. Pediatria n.a. G.N. Speransky. 2018;97(2):109-112. Available from: https://doi.org/10.24110/0031-403X-2018-97-2-109-112
- Volkova MN. Diseases of the oral mucosa: Educational and methodological manual. Vitebsk: VSMU; 2016;236. ISBN 978-985-466-848-2.
- Bechlau M, Madasio G, Oliveira J. Functional dysphonia: A strategy to improve patient outcomes. Patient Relat Outcome Meas. 2015;6:243-253. Available from: https://doi.org/10.2147/prom.s68631.
- Caffier F, Nawka T, Neumann K, Seipelt M, Caffier PP. Validation and classification of the 9-item Voice Impairment Index (VHI-9i). J Clin Med. 2021;10(15):3325. Available from: https://doi.org/10.3390/jcm10153325.
- Almeida N. Intelligent System for Diagnosing Pathologies in the Larynx Using Support Vector Machines. MSc thesis. Federal University Rio Grande do Norte; 2010. Available from: https://repositorio.ufrn.br/handle/123456789/15149.
- Liu X, Zheng Y, Yang J, Zou H. The impact of tonsillectomy with or without adenoidectomy on voice: acoustic and aerodynamic assessments. J Voice. 2015;29(3):346-348. Available from: https://doi.org/10.1016/j.jvoice.2014.08.014.
- Stepanova YE, Mokhotaeva MV, Korneenkov AA. Acoustic characteristics of the voice of representatives of vocal speech professions with functional dysphonia of the hypotonic type. Rossiiskaya otorinolaringologiya. 2021;20(4):58-63. Available from: http://dx.doi.org/10.18692/1810-4800-2021-4-58-63.
- Gorris C, Ricci Maccarini A, Vanoni F, Poggioli M, Vaschetto R, Garzaro M, et al. Acoustic analysis of normal voice patterns in Italian adults by using Praat. J Voice. 2020;34(6):961.e9-961.e18. Available from: https://doi.org/10.1016/j.jvoice.2019.04.016.
- Li G, Hou Q, Zhang C, Jiang Z, Gong S. Acoustic parameters for assessing voice quality in patients with voice disorders. Ann Palliat Med. 2021;10(1):130-136. Available from: https://doi.org/10.21037/apm-20-2102.
- Lopes LW, Batista Simões L, Delfino da Silva J, da Silva Evangelista D, da Nóbrega E, Ugulino AC, et al. Accuracy of acoustic analysis measurements in the evaluation of patients with different laryngeal diagnoses. J Voice. 2017;31(3):382.e15-382.e26. Available from: https://doi.org/10.1016/j.jvoice.2016.08.015.
- Alieva M, Nadzhmutdinova N, Abdukayumov A, Inoyatova F, Musaev M, Abdullaeva M. Spectral acoustic analysis of voice for diagnostics of dysphonia in children. In: Conceptual options for the development and improvement of medical science and psychology: collective monograph. Boston: Primedia eLaunch; 2023;6-13. Available from: https://isg-konf.com/wp-content/uploads/2023/06/Monograph/ISG.2023.MONO.MED.3/ISG.2023.MONO.MED.3.pdf.
- Jurca L, Vigaru C. Jitter and shimmer parameters in the identification of vocal tract pathologies. In: Proceedings of the 17th Acoustics and Vibration of Mechanical Structures—AVMS-2023, Timisoara, Romania, May 26-27, 2023. Springer Proceedings in Physics. 2023;302:155-164. Available from: http://dx.doi.org/10.1007/978-3-031-48087-4_17.
- Li G, Hou Q, Zhang C, Jiang C, Gona S. Acoustic parameters for assessing voice quality in patients with voice disorders. Ann Palliat Med. 2021;10(1):130-136. Available from: https://doi.org/10.21037/apm-20-2102.
- Starostina SV, Svistushkin VM, Rakunova EB. Postoperative voice rehabilitation in patients with benign and tumor-like diseases of the larynx according to acoustic analysis. Med Counc. 2019;(8):122-126. Available from: http://dx.doi.org/10.21518/2079-701X-2019-8-122-126.
- Wilson DK. Voice disorders in children. Translated from English by Nedvetsky AV. Moscow: Medicine; 1990;446.
- Afanasyev GI, Marchenko AV. Procedure of recording voice messages using Audacity program. Theory Pract Mod Sci. 2017;3(21):927-934.
- Ribeiro Fagundes RD, Russomano Th, Scolari D. Digital signal processing in the differential diagnosis of benign larynx diseases. Porto Alegre: Scientia Medica; 2006. 16(3):109-114.
- Teixeira JP, Gonçalves A. Accuracy of jitter and shimmer measurements. Procedia Technol. 2014;16(1):1190-1199. Available from: https://doi.org/10.1016/j.protcy.2014.10.134
- Wertzner HF, Schreiber S, Amaro L. Analysis of fundamental frequency, jitter, shimmer and voice intensity in children with phonological disorders. Rev Bras Otorhinolaringol. 2005;71:97-110. Available from: https://doi.org/10.1016/s1808-8694(15)31261-1
- Guimarães I. The science and art of the human voice. Alcoitão Higher School of Health; 2007;276. Available from: https://www.researchgate.net/publication/259892108_A_ciencia_e_a_arte_da_voz_humana