More Information
Submitted: February 03, 2025 | Approved: February 10, 2025 | Published: February 11, 2025
How to cite this article: Gregory C, Olivier L, Bourgeois P. Lymphoscintigraphic Investigations for Women with Lower Limb Edemas After One Pregnancy. Arch Case Rep. 2025; 9(3): 066-072. Available from:
https://dx.doi.org/10.29328/journal.acr.1001129
DOI: 10.29328/journal.acr.1001129
Copyright license: © 2025 Gregory C, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pregnancy; Lymphedema; Primary; Lymphoscintigraphy
Lymphoscintigraphic Investigations for Women with Lower Limb Edemas After One Pregnancy
Callebaut Gregory1, Leduc Olivier2 and Pierre Bourgeois1,3*
1Service of Vascular Surgery, HIS-IZZ Hospitals, Free University of Brussels, Brussels, Belgium
2Lympho-phlebology Unit, Department of Occupational and Environmental Physiology, Haute Ecole HE2B ISEK, Brussels, Belgium
3Department of Nuclear Medicine and Multi-disciplinary Clinic-Unit of Lymphology, Institute Jules Bordet, Free University of Brussels, Brussels, Belgium
*Address for Correspondence: Pierre Bourgeois, Service of Vascular Surgery, HIS-IZZ Hospitals, Université Libre de Bruxelles, Brussels, Belgium, Department of Nuclear Medicine and Multi-disciplinary Clinic-Unit of Lymphology, Institut Jules Bordet, Université Libre de Bruxelles, Brussels, Belgium, Email: [email protected]
Lower extremity edema is one of the most common complaints among pregnant patients. Lymphatic origin to these edemas is rarely considered and few cases of lymphedema after pregnancy have been reported and documented in medical literature. We describe here a series of 15 cases where the diagnosis of lymphedema was established by lymphoscintigraphy. Dermal reflux was observed in ten of the 15 patients (66%), popliteal lymph nodes in 11 (73%), and the edematous limb(s) were said to be abnormal in all but one case which showed only functional asymmetry at rest and limited vascular reflux in a calf.
Lower Extremity Edema (LEE) is one of the most common complaints among pregnant patients.
These edemas are related to increased water in the interstitial areas and their weekly prevalence increases significantly from 20% in the 31st week to 60% in the 42lnd gestational week [1]. They are usually symmetric, mild, and disappear after birth. However, these edemas can sometimes be severe and/or asymmetric and/or persist after gestation. If there is no evidence of venous problem at the level of the limb and/or in the pelvis, the hypothesis of one lymphatic disease must be raised. Such lymphedemas occurring during and/or after pregnancy have so far given rise to only a few case reports in the medical literature [2-8]. These situations are problematic for most doctors because the diagnosis is not without consequences. While they are familiar with so-called secondary lymphedemas (for example after trauma, after surgery, after cancer treatment,…), they are less familiar with such “idiopathic” edemas, also known as “primary lymphedemas”. We report in this article a series of cases of patients where such primary lymphedema after one or more pregnancies appeared and could be documented.
All medical data and information were obtained after informed consent and used in agreement with the rules of conduct dictated by the institutions, in agreement with the ethics committee (for Bordet, ethics committee number 2048; for HIS, ethics committee number CEHIS/2022-2).
Lymphoscintigraphy (LySc) for the lower limb edemas [9]
Our methodological protocol can be summarized as follows. 0.2 ml of 99mTc-labeled (74 MBq per injection) Human Serum Albumin nanosized colloids (0.05 mg per injection: Nanocoll® or NanoScint®) are injected subcutaneously (using tuberculin syringe) in the upper third of the first interdigital space of each foot the patient lying on the table of examination and having been informed that she had not to move the toes and feet during the following 30 minutes. Lymphoscintigraphies were conducted with an SMV ST-XLi from GE Healthcare (GE-Healthcare, Little Chalfont, United Kingdom) (Figures 1-8).
Figure 1: Case n° 3: Woman 41 years old who report temporary swelling in her left leg during her first pregnancy 14 years ago and then permanent bilateral swelling during her second pregnancy 3 years late (more marked on the left than on the right): her lymphoscintigraphic investigation was normal at the level of her right lower limb while lymphatic vascular reflux are seen on the left side extending from the inferior inguinal lymph nodes to the inner part of the thigh (« proximal dermal back flow » : see arrows).
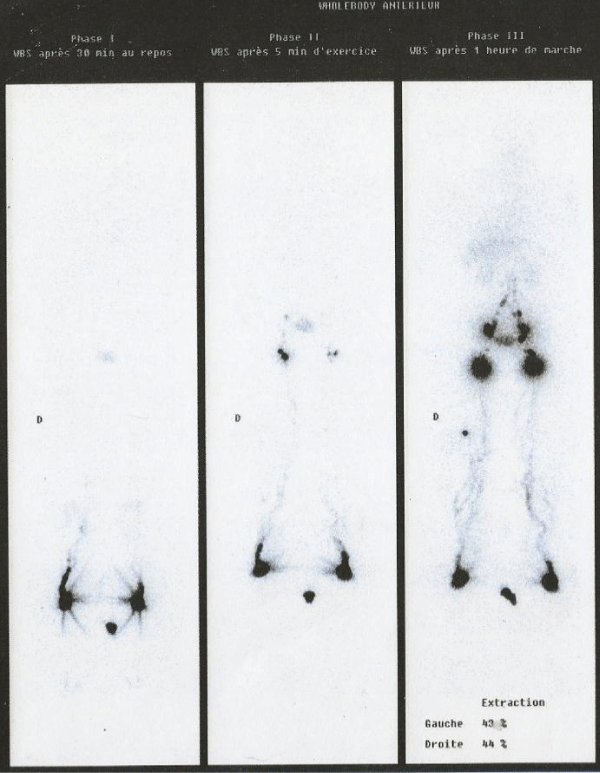
Figure 2: Case n° 4: Woman 45 years old with Left Lower Limb Edema manifesting transiently during her first pregnancy at the age of 32 years and also during the second 7 years ago but persisting non resolving since her third most recent pregnancy. Her phase 3 Lymphoscintigraphic investigation showed one « Lymph System » functional « hypoplasia » (more marked on the right side than in the left) with one bilateral distal dermal back at the level of the feet (and of the right ankle, also with popliteal LN).
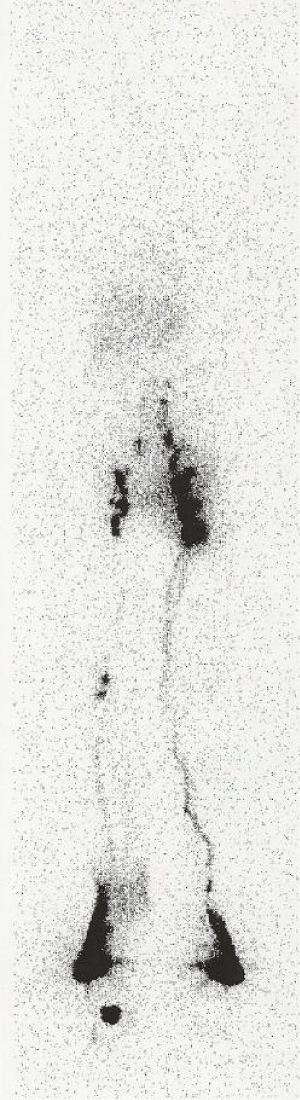
Figure 3: Case n° 6: Woman 33 years old with one bilateral lower limb edema during her first pregnancy four years ago but now Left>Right after her 2lnd pregnancy: her phase lymphoscintigraphic investigation (Figure 3) showed at the level of the left limb one segmental dermal backflow at the level of the foot see oblique arrow), one superficial lymph vessel aplasia (sLVA) with popliteal lymph nodes (see horizontal arrow) and inguinal lymph node aplasia (see white arrow: LNA).
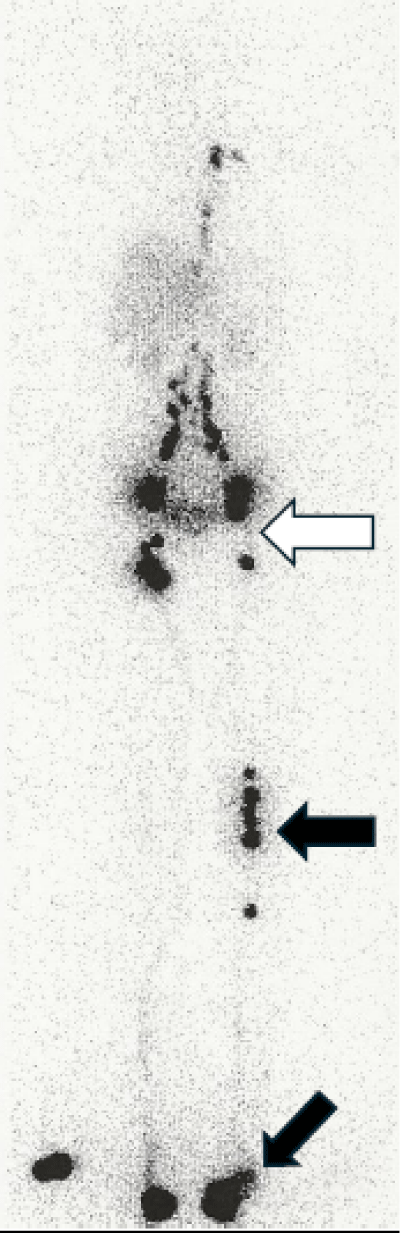
Figure 4: Case n° 7: woman 33 years old with one left lower limb edema since her third pregnancy 15 years ago: her phase 3 lymphoscintigraphic investigation showed one superficial lymph vessel hypoplasia with popliteal lymph nodes at the level of the left limb with distal dermal back flow at the level of her left foot and ankle..
Figure 5: Case n° 8: woman 48 years old with one left lower limb edema since her second pregnancy five years ago: her lymphoscintigraphic investigation showed on the right side one functional lymphatic insufficiency when compared to the left side (see left-sided Whole Body Scan: superficial lymph vessel hypoplasia) with popliteal lymph nodes appearing after phase 3 (see right-sided Whole Body Scan) but limited lymphatic Vascular Reflux (segmental DBF) being also observed after phase 3 at the level of the calf (see arrows on Figure 5).
Figure 6: Case n° 9: woman 46 years old with lower limb edemas since age 15 worsened after her pregnancy 5 years ago: her lymphoscintigraphic investigation (Figure 6) showed one bilateral lymph system functional hypoplasia (the tracer does not reach the inguinal lymph nodes) with at the level of the right limb, one superficial lymph vessel hypoplasia with popliteal lymph node (see horizontal arrow) and inguinal lymph node aplasia (see oblique arrow).
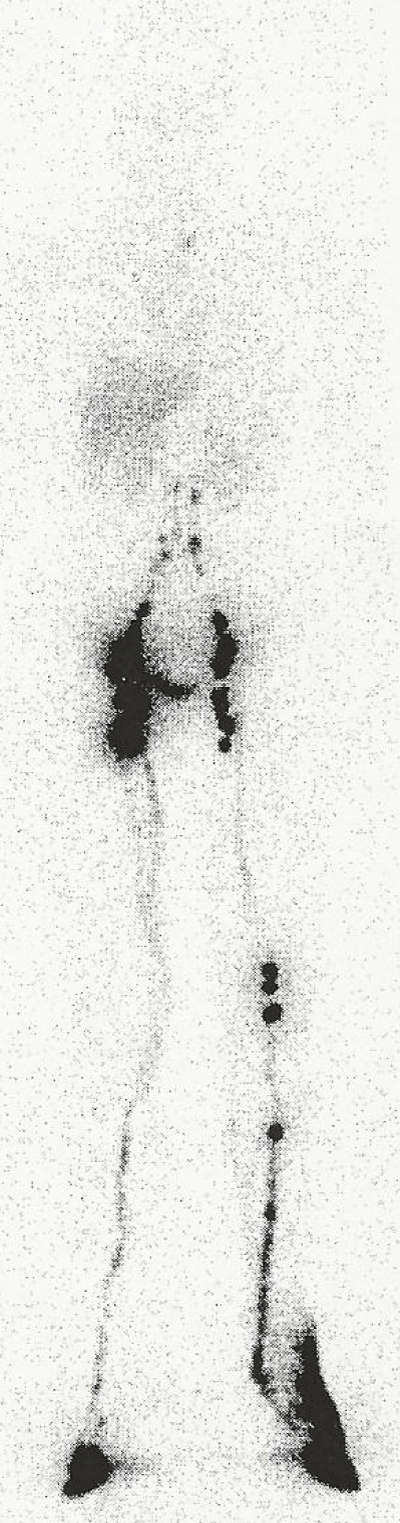
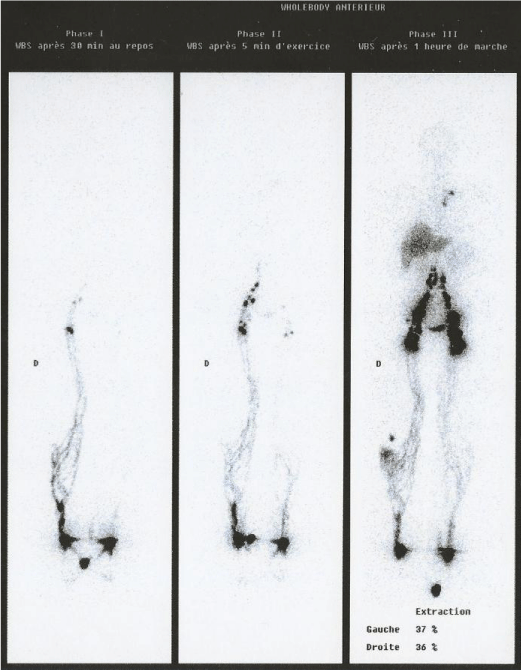
Figure 7: Case n° 13: woman 75 years old with left lower limb edema since her pregnancy at age 25: her phase 3 lymphoscintigraphic investigation (Figure 7) showed at the level of her left limb, one left lymph system functional hypoplasia with one superficial lymph vessel hypoplasia with popliteo-sural lymph nodes.
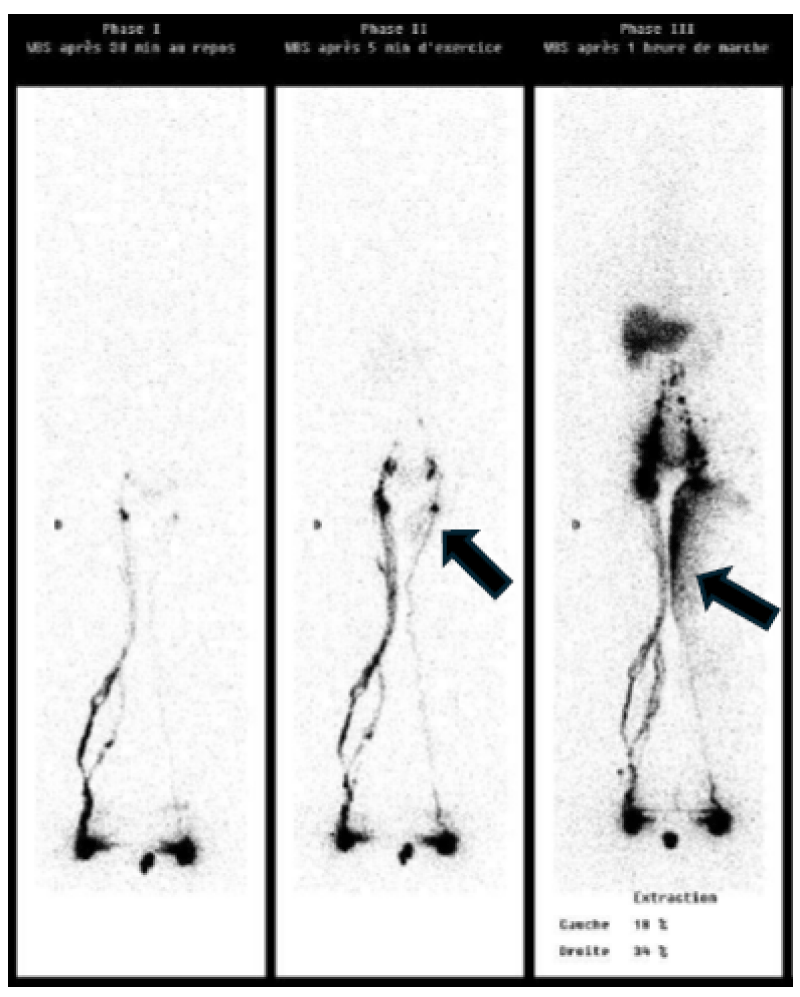
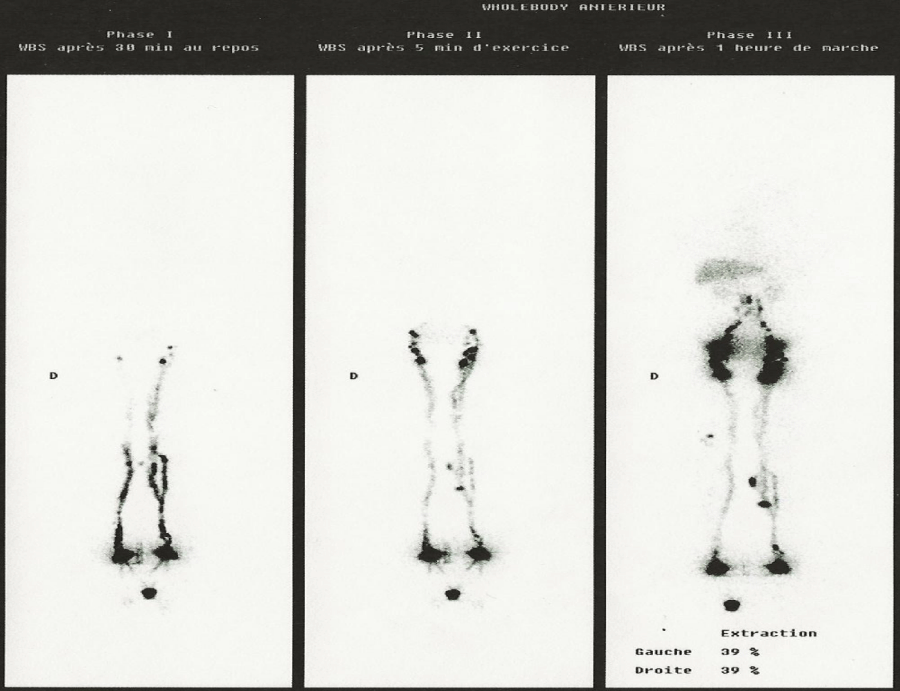
Figure 8: Case n° 1: woman 40 years old with recent post-partum right sided Lower Limb Lymph-Edema: her lymphoscintigraphic investigation showed on the left side one functional lymphatic insufficiency when compared to the right side (see left-sided and mid-sided Whole Body Scan (superficial lymph vessel hypoplasia) with popliteal lymph nodes appearing after phase 3 (see right-sided WBS) but left limited lymphatic Vascular Reflux (segmental Dermal Back-Flow) being also observed at the level of the calf on the right side (see arrows on Figure 8).
One static picture of the injected sites is obtained directly after the injections and thereafter the camera head is moved to the inguinal areas on which one dynamic imaging is performed (for 30 minutes) to see -in resting conditions- the time to inguinal nodes appearance and to evaluate the possible asymmetry in the nodal accumulation of the “tracer”.
One first whole-body imaging (anterior and posterior views) is thereafter obtained (this is our “phase 1”).
For “phase 2”, one dynamic imaging (lasting 15 minutes) is performed on the inguino-iliac areas but with the patient performing tip-toeing during the 15 minutes of the acquisition (the patient still lying on the table of examination and with the same goals as for “phase 1” but also to have one higher activity in the lymphatic vessels of the limbs).
One 2lnd whole body scan is thereafter systematically obtained as well as one 3rd after one hour of normal deambulation-activities (“phase 3”; see Figures 2-4,7). The injected sites are also imaged at the end of the exam to calculate the percent of radio-colloids extracted from the injected sites by the lymphatic system at the end of the investigation (normal values of extraction are equal to or higher than 30%).
The whole protocol lasted at most 3 hours (and was limited so that the patient was busy for only half a day: see Figures 1,5,6,8 showing three whole-body scans).
The qualitative analysis and description of the lymphoscintigraphic images:
The abnormal lymphatic situations detected on our examinations are as follows:
- The“proximal dermal backflows” (pDBF), i.e. images (Figure 1) where lymphatic vascular reflux (LVr) at the level of the root of the limb extends to the level of the superficial dermal network (true “DBF”) and progresses-descends distally until sometimes occurring, reflecting edema affecting the entire lower limb.
- The “distal dermal backflows” (dDBF), i.e. images (Figures 2,4) where LVr begins in the foot, extend to the level of the superficial dermal network to progress upward and until sometimes reflecting edema affecting the entire lower limb.
- The “Segmental Dermal Backflow-s” (sDBF), i.e. images (Figures 3,5,8) where LVr appears between these two extremities of the limb, extends generally to the level of the superficial dermal network and can progress proximally or distally until sometimes showing an edema affecting all or part of the lower limb.
- The Popliteal lymph nodes are frequently seen in patients with edema on their LySc (Figures 2-7).
- According to the classification adopted by the Belgian Society of Lymphology, the lymphatic system of one edematous limb is said morphologically and/or functionally “hypo-plastic” and/or “a-plastic” in the following situations:
- After interdigital injection, only deep lymphatic vessels (dLV) are seen at the level of the calf with intercalated lymph nodes, sometimes without inferior inguinal LN (Figure 3) è superficial lymph-angio-aplasia or sLVA,
- After interdigital injection, both deep and superficial LV are observed with popliteal and/or sural intercalated LN è “superficial and/or deep lymph-angio hypoplasia” or sLVH-dLVH,
- After interdigital injection, inguinal and/or iliac LN is not seen or hypoactive (Figure 6) : è “Lympho-Nodal-Aplasia” (or LNA) and “Lympho-Nodal-Hypoplasia” (or LNH),
- After interdigital injection, inguinal and iliac LN are well seen but pDBF is seen è “proximal Lympho-Nodal-Hypoplasia” (or pLNH),
- After interdigital injection, the tracer does not reach the inferior inguinal LN after phase 1 (Figure 8) and/or after phase 2 and/or extraction is decreased under the value of 30% and/or extractions, nodal accumulations of the tracer after phase 1 and/or 2 (Figure 8) show significant asymmetry è “Lymph-System-Hypoplasia” or LSH,
- After injection in the retro malleolar anterior space of the triceps surae tendon (Kager’s triangle), no deep lymph vessels are seen running deep in the calf: sometimes with increased lymph flow at the level of the superficial LV of the edematous limb when compared to the normal limb [10] è deep lymph-nodal « aplasia » or dLNA.
| Table 1: Demographic data of the 15 women in our analysis (2lnd column = age when LySc was performed: 3rd column = age of pregnancy when limb-edema was observed: 4th column = lateralisation of the limb-edema), with the results in terms of presence or not of dermal-back-flow (DBF? Bilaterally observed, only right sided or left sided), of popliteal lymph node (Pop LN?) and according to BeSL classification. | |||||||
| Case | LySc | LLE | Lat. | DBF? | Pop LN? | LySc Classification? | |
| 1 | 40 | 40 | bil | sDBF right calf | Right dLVH, left LSH | Figure 8 | |
| 2 | 25 | 25 | bil | sDBF bil calf | Bil | Bil sLVH | |
| 3 | 41 | 30 | L>R | pDBF left | Left pLNH | Figure 1 | |
| 4 | 44 | 32 | R | dDBF right | Right | Right sLVH, bil LSH | Figure 2 |
| 5 | 44 | 41 | L>R | dDBF bil | Bil | Bil sLVH, bil LSH | |
| 6 | 33 | 32 | L>R | sDBF left foot | Left | Left LSH-sLVA | Figure 3 |
| 7 | 47 | 32 | L>R | dDBF left | Left | Left LSH-sLVA | Figure 4 |
| 8 | 48 | 32 | L | sDBF left | Right | Right LSH? | Figure 5 |
| 9 | 46 | 41 | bil | Right | Bil LSH-LNA, right sLVH | Figure 6 | |
| 10 | 47 | 25 | Bil | Bil LSH | |||
| 11 | 36 | R>L | Right | Right LSH-sLVH | |||
| 12 | 54 | 20 | bil | dDBF left | Bil | Bil LSH-sLVH | |
| 13 | 75 | 25 | L | Left | Left LSH-sLVH | Figure 8 | |
| 14 | 43 | 22 | R | Right | Right sLVH | ||
| 15 | 37 | 22 | R>L | dDBF left | Bil LSH | ||
| sDBF = ”segmental dermal-back-flow” (and its localization, at the level of the foot or calf): pDBF= “proximal dermal-back-flow”; dDBF = “ distal dermal-back-flow”: LSH = Lymph System Hypoplasia: sLVH = superficial Lymph Vessel Hypoplasia: pLNH = proximal Lymph Node Hypoplasia: sLVA = superficial Lymph Vessel Aplasia: LNA = Lymph Node Aplasia. | |||||||
- Patient n° 1: woman 40 years old with recent post-partum right-sided Lower Limb Edema. Her lymphoscintigraphic investigation was abnormal at the level of her left Lower Limb (LL) with the tracer not reaching the inguinal lymph node after phase 1 (see left-sided WHS in Figure 8), lymph flow being decreased when compared to the right after phase 2 (see mid-sided WBS of Figure 8) and with lymphatic vascular reflux appearing after phase 3 at the level of the calf (« segmental dermal backflow »: see arrow on right-sided WBS of Figure 8).
- Patient n° 2: woman with bilateral LLLE since the age of 26 years after her last pregnancy with bilateral segmental dermal backflow at the level of the calf on her LySc.
- Patient n° 3: woman 41 years old who reported temporary swelling in her left leg during her first pregnancy 14 years ago and then permanent bilateral swelling during her second pregnancy 3 years later (more marked on the left than on the right). Her lymphoscintigraphic investigation was normal at the level of her right Lower Limb (LL) while lymph flow was decreased at the level of the left LL when compared to the right after phase 1 (see right-sided WBS of Figure 1), also with lymphatic vascular reflux being observed on the left side extending from the inferior inguinal lymph nodes to the inner part of the thigh (« proximal dermal backflow »: see arrows on Figure 1).
- Patient n° 4: woman 45 years old with Left Lower Limb Edema manifesting transiently during her first pregnancy at the age of 32 years and also during the second 7 years ago but persisting nonresolving since her third most recent pregnancy. Her phase 3 Lymphoscintigraphic investigation (Figure 2) showed one « Lymph System » functional « hypoplasia » (more marked on the right side than on the left) with one bilateral distal dermal back at the level of the feet (and of the right ankle, also with popliteal LN).
- Patient n° 5: woman 44 years old with post-partum lower limb edemas since her pregnancy three years ago: her lymphoscintigraphic investigation showed bilaterally one “superficial lymphangioma- hypoplasia” (sLVA) with one -bilateral- distal dermal backflow, deep popliteal lymph nodes, and one right inguinal lymph node hypoplasia.
- Patient n° 6: woman 33 years old with one bilateral lower limb edema during her first pregnancy four years ago but now Left>Right after her 2lnd pregnancy: her phase lymphoscintigraphic investigation (Figure 3) showed at the level of the left limb one segmental dermal backflow at the level of the foot, one superficial lymph vessel aplasia (sLVA) with popliteal lymph nodes and inguinal lymph node aplasia (LNA).
- Patient n° 7: woman 33 years old with one left lower limb edema since her third pregnancy 15 years ago: her phase 3 lymphoscintigraphic investigation (Figure 4) showed one superficial lymph vessel hypo plasia with popliteal lymph nodes at the level of the left limb with distal dermal backflow at the level of her left foot and ankle.
- Patient n° 8:: woman 48 years old with one left lower limb edema since her second pregnancy five years ago: her lymphoscintigraphic investigation showed on the right side one functional lymphatic insufficiency when compared to the left side (see left-sided WBS in Figure 5: superficial lymph vessel hypoplasia) with popliteal lymph nodes appearing after phase 3 (see right-sided WBS) but limited lVR (segmental DBF) being also observed after phase at the level of the calf on the left side (see arrows on Figure 5).
- Patient n° 9: woman 46 years old with lower limb edemas since age 15 worsened after her pregnancy 5 years ago: her lymphoscintigraphic investigation (Figure 6) showed one bilateral lymph system functional hypoplasia at the level of the right limb, one superficial lymph vessel hypoplasia with popliteal lymph node and inguinal lymph node aplasia (see arrows).
- Patient n° 10: Patient 47 years old, referred for evaluation of lymphangiopathy for 20 years, with lower limb edema after her first pregnancy at age 25, its stabilization before aggravation 4 years ago: her lymphoscintigraphic investigation showed one bilateral lymph system functional hypoplasia.
- Patient n° 11: woman 36 years old with lower limb edemas right>left after pregnancy: her lymphoscintigraphic investigation showed one right lymph system functional hypoplasia with superficial lymph vessel hypoplasia and popliteal lymph node.
- Patient n° 12: woman 54 years old with bilateral lower limb edema since her first pregnancy at age 20: her lymphoscintigraphic investigation showed one left lymph system functional hypoplasia, one bilateral superficial lymph vessel hypoplasia with popliteal lymph nodes, and one distal dermal backflow at the level of her left foot.
- Patient n° 13: woman 75 years old with left lower limb edema since her pregnancy at age 25: her phase 3 lymphoscintigraphic investigation (Figure 7) showed at the level of her left limb, one left lymph system functional hypoplasia with one superficial lymph vessel hypoplasia with popliteo-sural lymph nodes.
- Patient n° 14: woman 43 years old with lower limb edema since her second pregnancy at age 22: her lymphoscintigraphic investigation showed one right lymph vessel hypoplasia with popliteal lymph node.
- Patient n° 15; woman 37 years old with edema right>left since her first pregnancy: her lymphoscintigraphic investigation showed one bilateral lymph system functional hypoplasia with one left distal dermal backflow at the level of the foot.
Dermal reflux was observed in ten of the 15 patients (66%), popliteal lymph nodes in 11 (73%), and the edematous limb(s) were said to be abnormal in all but one case (case 8: Figure 5) which showed only functional asymmetry at rest and limited vascular reflux (sDBF) in a calf.
By itself, pregnancy may be considered as a situation meeting all conditions « forcing » and favoring the appearance of previously latent and asymptomatic lymphatic insufficiencies and/or disease, of one “primary” lymphedema:
- The hormonal « climate » of pregnancy can lead to physiological edema due to sodium retention.
- Hypertension sometimes associated with pregnancy may also increase the risk of having lower-extremity edema, especially if there is insufficient venous return.
- Edema can also occur because the gravid uterus compresses the inferior vena cava and the iliac veins during recumbency, obstructing the return of the femoral veins.
- Deep vein thrombosis is also more common during pregnancy because it induces a hypercoagulable state and because women are less mobile.
Unilateral edema at the level of the leg, calf, or foot with or without warmth, redness, or tenderness, or fever represents thus « warning » sign. If a venous problem can be then easily ruled out by Doppler ultrasonography (US), the possibility of involvement-disease of the lymphatic vessels and/or nodes should be considered if the US exam is normal.
Primary lymphedemas are considered a rare disease. Their prevalence is estimated at 1.5 per 100.000 people younger than 20 in an old, retrospective study [11], most likely underestimating this figure [12]. When these lymphedematous situations are diagnosed “late”, they represent a progressive, chronic, and sometimes serious “disease” that can and should be managed [13].
The imaging techniques for the diagnosis of the Lymphatic Lower Limb Edema (LLLE)
Three techniques may be proposed to demonstrate the lymphatic character of such edema and to image lymphatic vessels and lymph nodes [13-24].
T2 weighted Magnetic Resonance Imaging with fat suppression [16,24] allows us to visualize very small LV and their abnormalities but is expansive and sometimes difficult to access. Because of its resolution, its relative simplicity of implementation, and its (relative) low cost, Near Infrared fluorescence imaging of the Lymphatic Vessels (LV) and Lymph Nodes) (LN) after injection of Indocyanine Green (ICG) (NIFRLI) is now increasingly being proposed for the assessment of the limb edemas [17-19] but is limited by photon scatter and absorption in the tissue which restricts imaging to the superficial LV (to a depth of 1 cm). Lympho-scintigraphy (LySc) is generally considered the standard test to image the lymphatic vessels and lymph nodes of the lower limbs after injection of 99mTc radiolabeled nanosized colloids [20-24]. However, because of its radiant nature and the appearance of the isotope in breast milk, LySc can only be performed after pregnancy when the woman is no longer breast-feeding and when the child (and children) can be kept away from the mother for 72 hours after the injections.
Dermal backflows in the medical literature
For the 3 techniques, the diagnosis of lymphedema is based on the demonstration of dermal reflux of the “tracer”, also called “dermal backflow” (DBF), which appeared in the medical literature devoted to lymphatic vessel imaging of lymphedematous situations as early as 1955 with radiological lymphography [25,26].
The authors distinguished from the outset:
- Proximal reflux (pDBF) following lymph node excision and associated treatments (2ary) and/or congenital lymph-adenoplasia (1ary) and/or progressive fibrosis of the inguinal and/or intra-abdominal lymph node structures
- Distal reflux (dDBF) following lymphangio-hypo or aplasia of the distal lymphatic vessels (initial and/or pre-collector and/or collector) in patients who here develop edema that begins in the foot and progresses to the root of the limb.
Between these two extreme developments, sDBFs are considered by Browse [27] to be “acquired” (rather than congenital) and linked to lymphangio-obliterative phenomena by the development of intraluminal or intramural thrombosis of lymphatic vascular segments. They can be seen in combination with the previous two.
Proximal dermal back flows were reported in 16 % of the patients and dDBF in 24% with 1ary LLLE by Wolfe and kinmonth. In our small series, pdbf was observed in one woman (/15), ddbf in five (/15) and sDBF in four (/15).
The popliteal lymph nodes (popLN)
In this small series of 15 cases, popliteal LN is observed in 11 patients. Their visualization reflects a functional insufficiency of the superficial lymphatic network, a compensatory phenomenon where the lymphatic load is partly or diverted to the deep network [28].
Potential implications of a diagnosis of primary lymphedema after pregnancy
While the vast majority of primary lymphedemas are “sporadic” and can be considered “benign”, they are sometimes reported by patients as “congenital” and/or present in the families and genetic abnormalities should be sought [29]. Indeed, these may be autosomal dominant but also recessive. The distinction between these two situations when diagnosed after a first pregnancy is not without consequences for possible subsequent ones. While these situations must not be underestimated, they also must not be overestimated and give rise to the impression of a “disaster” among the patients and families concerned.
The occurrence of edema during or following pregnancy, the origin of which may be suspected of lymphatic and being “primary” (if not “congenital” in a family context) does not seem so rare. Lymphoscintigraphy of the lower extremities is one way to make this diagnosis and should be proposed to women presenting such edematous situations, especially when persisting after pregnancy and/or affecting, either one limb, or both limbs but asymmetrically, and when a venous problem has been ruled out by Doppler ultrasonography.
- Lebech M, Hansen M, Knudsen A. Headache, fatigue and edema of the lower limbs during the third trimester of normal pregnancy. Ugeskr Laeger. 1996;158(47):6778-80. Available from: https://pubmed.ncbi.nlm.nih.gov/8992699/
- Horn B, Kiszel J. Milroy-Nonne-Meige disease observed in a pregnant woman. Zentralbl Gynakol. 1964;86:317-21.
- Cantegrel C. A case of acute lymphedema during the 6th month of pregnancy. Phlebologie. 1972;25(3):287-90. Available from: https://pubmed.ncbi.nlm.nih.gov/4662056/
- Aronsson A, Roscher I. Lymphoedema of the inner thighs in late pregnancy. Acta Derm Venereol. 1997;77(3):249. Available from: https://doi.org/10.2340/0001555577249
- Biswas A, Kanti Kundu M, Kyal A, Ganguly RP, Sanyal P, Bhansali S, et al. Unilateral lower limb oedema in pregnancy. J Indian Med Assoc. 2007;105(10):598, 600, 602. Available from: https://pubmed.ncbi.nlm.nih.gov/18383955/
- Helwani MA, Donnelly JA, Makan M, De Wet CJ. A pregnant woman in the third trimester diagnosed with acute respiratory failure and severe lower-extremity edema. Chest. 2016;150(4):e105-e107. Available from: https://doi.org/10.1016/j.chest.2016.03.066
- Ochalek K. Three-year follow-up of the compression use in lower limb edema during pregnancy: A case report. J Vasc Nurs. 2021;39(2):43-46. Available from: https://doi.org/10.1016/j.jvn.2021.04.002
- Morimoto K, O’Rourke L. Third trimester lower extremity lymphorrhea. Case Rep Obstet Gynecol. 2021;2021:3594923. Available from: https://doi.org/10.1155/2021/3594923
- Bourgeois P. Methodological protocol for lymphoscintigraphy in limb edema. Belnuc 1–16. 2017. Available from: https://www.belnuc.be/news-test/
- Barbieux R, Roman MM, Rivière F, Leduc O, Leduc A, Bourgeois P, Provyn S. Scintigraphic investigations of the deep and superficial lymphatic systems in the evaluation of lower limb oedema. Sci Rep. 2019;9(1):13691. Available from: https://www.nature.com/articles/s41598-019-49554-7
- Smeltzer DM, Stickler GB, Schirger A. Primary lymphedema in children and adolescents: a follow-up study and review. Pediatrics. 1985;76(2):206-18. Available from: https://pubmed.ncbi.nlm.nih.gov/4022694/
- Brouillard P, Witte MH, Erickson RP, Damstra RJ, Becker C, Quéré I, et al. Primary lymphoedema. Nat Rev Dis Primers. 2021;7(1):77. Available from: https://doi.org/10.1038/s41572-021-00309-7
- Executive Committee of the International Society of Lymphology. The Diagnosis and Treatment of Peripheral Lymphedema: 2023 Consensus Document of The International Society of Lymphology. Lymphology. 2023;56(4):133-151. Available from: https://pubmed.ncbi.nlm.nih.gov/39207406/
- Vargo M, Aldrich M, Donahue P, Iker E, Koelmeyer L, Crescenzi R, et al. Current diagnostic and quantitative techniques in the field of lymphedema management: a critical review. Med Oncol. 2024;41(10):241. Available from: https://link.springer.com/article/10.1007/s12032-024-02472-9
- Markarian B, Toro C, Moreira K, Polam S, Mathew N, Mayrovitz HN. Assessment modalities for lower extremity edema, lymphedema, and lipedema: A scoping review. Cureus. 2024;16(3):e55906. Available from: https://doi.org/10.7759/cureus.55906
- Salehi BP, Sibley RC, Friedman R, Kim G, Singhal D, Loening AM, et al. MRI of lymphedema. J Magn Reson Imaging. 2023;57(4):977-991. Available from: https://doi.org/10.1002/jmri.28496
- Unno N, Inuzuka K, Suzuki M, Yamamoto N, Sagara D, Nishiyama M, et al. Preliminary experience with a novel fluorescence lymphography using indocyanine green in patients with secondary lymphedema. J Vasc Surg. 2007;45(5):1016-21. Available from: https://doi.org/10.1016/j.jvs.2007.01.023
- Han CY, Choi SH, Chi SH, Hong JH, Cho YE, Kim J. Nano-fluorescence imaging: advancing lymphatic system disease and monitoring. Nano Converg. 2024;11(1):53. Available from: https://nanoconvergencejournal.springeropen.com/articles/10.1186/s40580-024-00462-1
- Sevick-Muraca EM, Fife CE, Rasmussen JC. Imaging peripheral lymphatic dysfunction in chronic conditions. Front Physiol. 2023;14:1132097. Available from: https://doi.org/10.3389/fphys.2023.1132097
- Bourgeois P. Critical analysis of the literature on lymphoscintigraphic investigations of limbedemas. Eur J Lymphol Relat Probl. 1997;VI/21:1-21.
- Bourgeois P, Munck D, Becker C, Leduc O. Evaluation of a three-phase lymphoscintigraphic investigation protocol of the lower limbedemas. Eur J Lymphol Relat Probl. 1997;VI/21:22-28. Available from: https://www.researchgate.net/publication/292855898_A_three-phase_lymphoscintigraphic_investigation_protocol_for_the_evaluation_of_lower_limbedemas
- Szuba A, Shin WS, Strauss HW, Rockson S. The third circulation: radionuclide lymphoscintigraphy in the evaluation of lymphedema. J Nucl Med. 2003;44(1):43-57. Available from: https://pubmed.ncbi.nlm.nih.gov/12515876/
- Bourgeois P. Lymphoscintigraphy and other imaging methods. In: Green AK, Slavin SA, Brörson H, editors. Lymphedema: presentation, diagnosis, and treatment. Springer; 2015. Available from: https://doi.org/10.1371/journal.pone.0253900
- Quartuccio N, Agugliaro F, Alongi P, Sturiale L, Arnone G, Corrao S. A systematic review comparing lymphoscintigraphy and magnetic resonance imaging techniques in the assessment of peripheral lymphedema. Curr Med Imaging. 2022;19(5):469-475. Available from: https://doi.org/10.2174/1573405618666220525141721
- Kinmonth JB, Taylor GW, Harper RK. Lymphangiography: a technique for its clinical use in the lower limb. Br Med J. 1955;1(4919):940-2. Available from: https://doi.org/10.1136/bmj.1.4919.940
- Kinmonth JB, Taylor GW, Tracy GD, Marsh JD. Primary lymphoedema: clinical and lymphangiographic studies of a series of 107 patients in which the lower limbs were affected. Br J Surg. 1957;45(189):1-9. Available from: https://doi.org/10.1002/bjs.18004518902
- Browse NL, Stewart G. Lymphoedema: pathophysiology and classification. J Cardiovasc Surg (Torino). 1985;26(2):91-106. Available from: https://pubmed.ncbi.nlm.nih.gov/3884629/
- Burnand KM, Glass DM, Sundaraiya S, Mortimer PS, Peters AM. Popliteal node visualization during standard pedal lymphoscintigraphy for a swollen limb indicates impaired lymph drainage. AJR Am J Roentgenol. 2011;197(6):1443-8. Available from: https://doi.org/10.2214/ajr.11.6631
- Schlögel MJ, Brouillard P. Genetic causes of lymphedema. In: Greene AK, Slavin SA, Brorson H, editors. Lymphedema: presentation, diagnosis, and treatment. Springer Int Publ AG; Switzerland. Available from: https://link.springer.com/book/10.1007/978-3-319-14493-1