More Information
Submitted: March 20, 2025 | Approved: March 26, 2025 | Published: March 27, 2025
How to cite this article: Vázquez-Moreno J, Salazar-Nava RG, Velásquez-Pérez L. Mycobacterium colombiense in a Mexican Patient with HIV Identified by DNA Sequencing. Arch Case Rep. 2025; 9(3): 132-134. Available from:
https://dx.doi.org/10.29328/journal.acr.1001133
DOI: 10.29328/journal.acr.1001133
Copyright license: © 2025 Vázquez-Moreno J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Mycobacterium colombiense; Human immunodeficiency virus; Nontuberculous mycobacteria; Bone marrow aspirate; Molecular tests
Mycobacterium colombiense in a Mexican Patient with HIV Identified by DNA Sequencing
Jaime Vázquez-Moreno, Rosa Guadalupe Salazar-Nava and Leora Velásquez-Pérez*
Department of Epidemiology, National Institute of Neurology and Neurosurgery, Mexico City, Zip code 14269, Mexico
*Address for Correspondence: Leora Velásquez-Pérez, Ph.D, Department of Epidemiology, National Institute of Neurology and Neurosurgery, Mexico City, 3877, La Fama, Tlalpan ZC 14269, Mexico, Email: [email protected]
Mycobacterium colombiense is a rare nontuberculous mycobacterium (NTM) belonging to the Mycobacterium avium complex (MAC), primarily associated with respiratory disease. We report the case of a 39-year-old male from Mexico City, diagnosed with stage 4 Human Immunodeficiency Virus (HIV), in whom Mycobacterium colombiense was isolated from bone marrow using DNA sequencing, in the absence of pulmonary involvement . This represents the first documented case of Mycobacterium colombiense isolation in Mexico. Given that NTM cultures often require 2 to 3 weeks to yield results , diagnosis is often delayed, underscoring the importance of implementing molecular testing for prompt diagnosis and timely treatment initiation.
Mycobacterium colombiense is a slow-growing nontuberculous mycobacterium (NTM) that primarily affects immunocompromised individuals [1]. NTMs are opportunistic pathogens commonly found in water, soil, and dust [2,3]. First isolated in 2006 from HIV-positive patients, M. colombiense most frequently manifests as pulmonary disease (65% - 90%) [4]. Diagnosis is based on the presence of signs and symptoms and the isolation of the mycobacterium. In such infections, CD4 T lymphocyte counts are typically below 50 cells/mm³.
M. colombiense can be isolated from blood cultures, lymphatic fluid, bone marrow, or other body fluids. Detection has improved with molecular diagnostic techniques [1,5]. This is the first case report of M. colombiense in Mexico.
A 40-year-old man living with HIV was referred from the Condesa Specialized Clinic to the National Institute of Neurology and Neurosurgery (NINN) due to epileptic seizures. Forty days before hospital admission, he experienced abdominal pain, diarrhea, vomiting, fever (38 °C), myalgias, arthralgias, fatigue, severe headache, and a 12 kg weight loss over one month. He was treated with gentamicin and moxifloxacin for five days, without improvement . Subsequently, he developed tonic-clonic seizures with loss of consciousness, hypersalivation, and urinary incontinence.
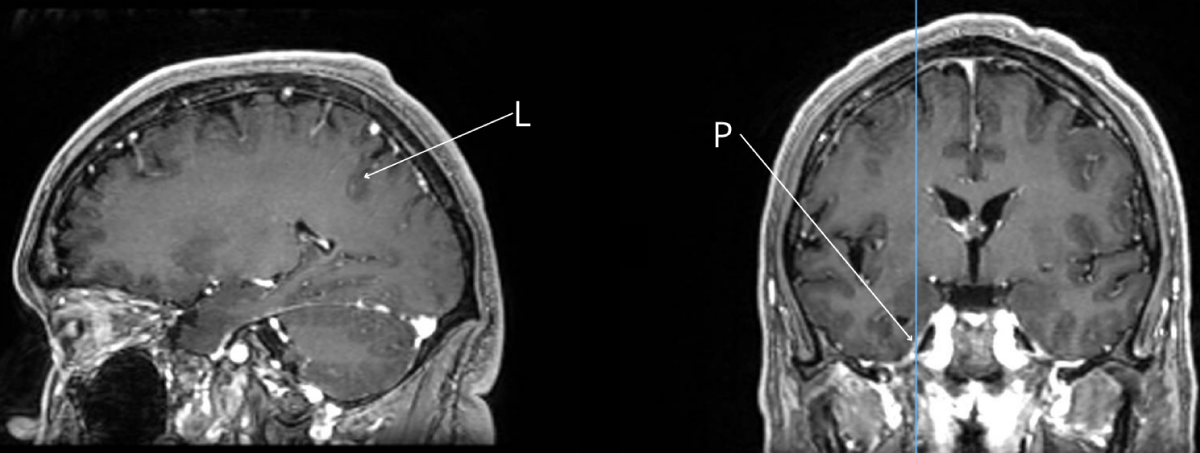
Upon admission to NINN, he presented sixth cranial nerve impairment and meningeal signs. Cranial, thoracic, and abdominal CT scans showed no abnormalities. A lumbar puncture revealed hypoglycorrhachia (26mg/dL), hyperproteinorrachia (76 mg/dL), hypocellularity (1.0 cells/mm³), and the presence of Cryptococcus was observed ; therefore, a Chinese ink test was performed with a positive result. CD4 count was 6 cells/mm³, and viral load was 241,219 copies/mL. Treatment was initiated with brivaracetam, levetiracetam, and fluconazole; Indian ink staining and FilmArray were positive for Cryptococcus neoformans . A central venous catheter was placed for administration of liposomal amphotericin B and trimethoprim/sulfamethoxazole . Brain MRI showed pachymeningeal and leptomeningeal enhancement (Figure 1). On hospital day six, hypokalemia (3.15 mEq/L) was detected, and potassium replacement was started.
Figure 1: Brain MRI Paquimenigitis (P) and leptominingitis (L) in a patient with M. colombiense.
On day 10, the patient developed pancytopenia, a bone marrow aspirate was performed on day 13 for bacterial, mycobacterial, and fungal cultures, along with special stains. On day 21, Histoplasma spp. was identified in cultures incubated at room temperature (< 24 °C) on Sabouraud agar.
By day 27, the patient experienced fever (38 °C), neurological deterioration, and leukocytosis, necessitating intensive care admission. He required vasopressors, sedation, and invasive airway support. Thoracic CT revealed bilateral basal infiltrates, leading to empiric treatment with vancomycin, meropenem, and tigecycline. He subsequently developed multiorgan failure and acute kidney injury, requiring renal replacement therapy and red blood cell transfusions (Hb 6.47 g/dL) due to hemolysis. Klebsiella spp. was isolated from both central and peripheral blood cultures, leading to antibiotic adjustments.
On day 36, invasive mechanical ventilation was withdrawn, and vasopressors were discontinued. On day 43; the patient developed fever, myopathy and erosions of the lips and oral mucosa. A multidrug empiric regimen was initiated including rifampicin, ethambutol, pyrazinamide, isoniazid, and clarithromycin. The following day, mycobacterial culture reported Mycobacterium spp.
On day 48, he developed lower gastrointestinal bleeding and hypovolemic shock. Despite multiple transfusions, he remained hemodynamically unstable and experienced cardiac arrest.
M. Colombiense was confirmed by full DNA sequencing thirteen days after death.
The isolation and reporting of M. colombiense is extremely rare and often overlooked by healthcare personnel [3]. The identification of NTM can be performed using various techniques, including Polymerase Chain Reaction (PCR)-based assays, high-performance liquid chromatography, and full genome sequencing [1].
This case, like most, involved a patient with severe immunosuppression due to HIV, with CD4 T lymphocyte counts <50 cells/mm³ . Unlike previous reports, this case did not predominantly involve the lungs, and alkaline phosphatase levels remained normal. However, cases in immunocompetent individuals have been reported, such as one described in Brazil in 2016 [6].
Most NTM infections are diagnosed late. These mycobacterial cultures typically require 2 to 3 weeks to grow , highlighting the importance of molecular testing for prompt diagnosis and timely treatment initiation, thus improving the prognosis of the disease [7].
M. colombiense is a rare opportunistic pathogen. We report the first case of its isolation in Mexico, confirmed through DNA sequencing performed on a bone marrow aspirate. Delayed diagnosis is common due to its rarity and the nonspecific nature of clinical manifestations in immunocompromised individuals.
Clinicians should maintain a high index of suspicion for MAC infections even in the absence of classic symptoms, particularly in immunocompromised patients who fail to respond to conventional treatment. However, the cost and limited availability of advanced molecular diagnostics restrict their use in many healthcare settings.
We thank the patient’s family for their consent to publish this case report.
Ethical considerations
As the definitive diagnosis of Mycobacterium colombiense was obtained postmortem, authorization for publication was requested from the patient’s family. The case is presented with strict adherence to confidentiality and ethical standards.
CRediT authorship contribution statement
- Jaime Vázquez-Moreno: Writing – original draft, review and editing.
- Rosa Guadalupe Salazar-Nava: Review.
- Leora Velásquez-Pérez: Writing - review and editing, Validation.
- Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents With HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. National Institutes of Health, HIV Medicine Association, and Infectious Diseases Society of America. Available from: https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-opportunistic-infection
- Falkinham J. Environmental sources of nontuberculous mycobacteria. Clin Chest Med. 2015;36(1):35-41. Available from: https://doi.org/10.1016/j.ccm.2014.10.003
- Andreani J, Barrassi L, Davopust B, La Scola B. Evidence of an environmental reservoir for emergent Mycobacterium colombiense. New Microbes New Infect. 2020;35:100666. Available from: https://doi.org/10.1016/j.nmni.2020.100666
- Yu X, Jiang W. Mycobacterium colombiense and Mycobacterium avium complex causing severe pneumonia in a patient with HIV identified by a novel molecular-based method. Infect Drug Resist. 2021;14:11-6. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7797356/
- Tang M, Zeng W, Qiu Y, Fang G, Pan M, Li W, et al. Clinical features of rare disseminated Mycobacterium colombiense infection in nine patients who are HIV-negative in Guangxi, China. Int J Infect Dis. 2023;128:321-4. Available from: https://pubmed.ncbi.nlm.nih.gov/36642210/
- Barretto AR, Felício JS, Sales LHM, Yamada ES, Lopes ML, da Costa ARF. A fatal case of pulmonary infection by Mycobacterium colombiense in Para State, Amazon Region, Brazil. Diagn Microbiol Infect Dis. 2016;85(3):344-6. Available from: https://doi.org/10.1016/j.diagmicrobio.2016.02.011
- Pennington K, Vu A, Challener D, Rivera CG, Shweta FNU, Zeuli JD, et al. Approach to the diagnosis and treatment of non-tuberculous mycobacterial disease. J Clin Tuberc Other Mycobact Dis. 2021;24. Available from: https://doi.org/10.1016/j.jctube.2021.100244