More Information
Submitted: April 03, 2025 | Approved: April 09, 2025 | Published: April 10, 2025
How to cite this article: Babbiker IM, Elimam AMA, Medani IE, Omar AI. Uterine Fibroid Causing Acute Abdomen Due to Ischemic Gangrene: A Case Report. Arch Case Rep. 2025; 9(4): 140-141. Available from:
https://dx.doi.org/10.29328/journal.acr.1001135
DOI: 10.29328/journal.acr.1001135
Copyright license: © 2025 Babbiker IM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Uterine fibroids; Pedunculated fibroid; Ischemic gangrene; Acute a bdomen
Uterine Fibroid Causing Acute Abdomen Due to Ischemic Gangrene: A Case Report
Isam Mohamed Babbiker1, Ali Mohammed Ali Elimam2*, Isameldin Elamin Medani3 and Abdalmuein Ibrahim Omar4
1Assistant Professor, Obstetrics and Gynecology Department, University of Sinnar, Sudan
2Assistant Professor, Obstetrics and Gynecology Department, Elneelain University, Sudan
3Obstetrician and Gynecologist, Jazan University, College of Medcine, Saudi Arabia
4Assistant Professor, Obstetrics and Gynecology Department, Shendi University, Sudan
*Address for Correspondence: Dr. Ali Mohammed Ali Elimam, Assistant Professor, Obstetrics and Gynecology Department, Elneelain University, Sudan, Email: [email protected]
Our case report discusses the importance of a rare presentation (twisted fibroid) causing severe abdominal pain and the diagnostic dilemma, which may result in ischemic gangrene, increasing morbidity and mortality.
Again, it highlights the correlation between clinical picture and radiological findings, the important technical points when doing ultrasound for pelvic mass and its impact on management plan. The collaboration between the gynecologist and radiologist, along with timely intervention, leads to better outcomes.
Uterine fibroids are common tumors in women in reproductive age. They are commonly found asymptomatic, but can cause heavy periods, heaviness, pressure symptoms, infertility, and rarely emergency conditions like in our case.
Acute abdomen related to uterine fibroid is rare, but failure to diagnose the condition can lead to serious complications such as ischemic gangrene and peritonitis.
Our case sheds light on the difficulty to diagnose ischemic gangrene of pedunculated uterine fibroid as the radiological findings are non-specific. Degeneration of uterine fibroid is known to occur during pregnancy, after Uterine Artery Embolization (UAE), and during menopause.
Degeneration of uterine fibroid occurs secondary to a loss of blood supply and is usually attributed to rapid growth associated with pregnancy. Pain is the most frequent sign of uterine leiomyoma degeneration [1] but it’s not specific in nature to degeneration of leiomyoma and this may lead to confusion in diagnoses and so delay the management.
The incidence of cystic degeneration of uterine fibroid is 4% and is more in post-menopausal women and fibroids of interstitial type [2]. This fact explains why such condition can be misdiagnosed in clinical practice.
22-year-old single woman suffering from recurrent abdominal pain and tenderness. Evaluated and treated at local clinic many times with no response. She came to Emergency Room (ER) with nausea, vomiting, and severe abdominal pain.
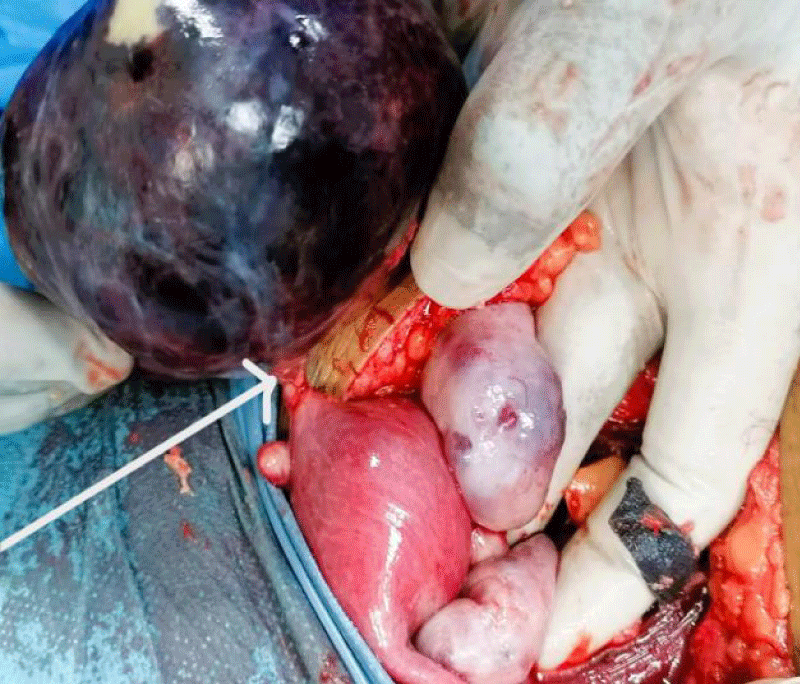
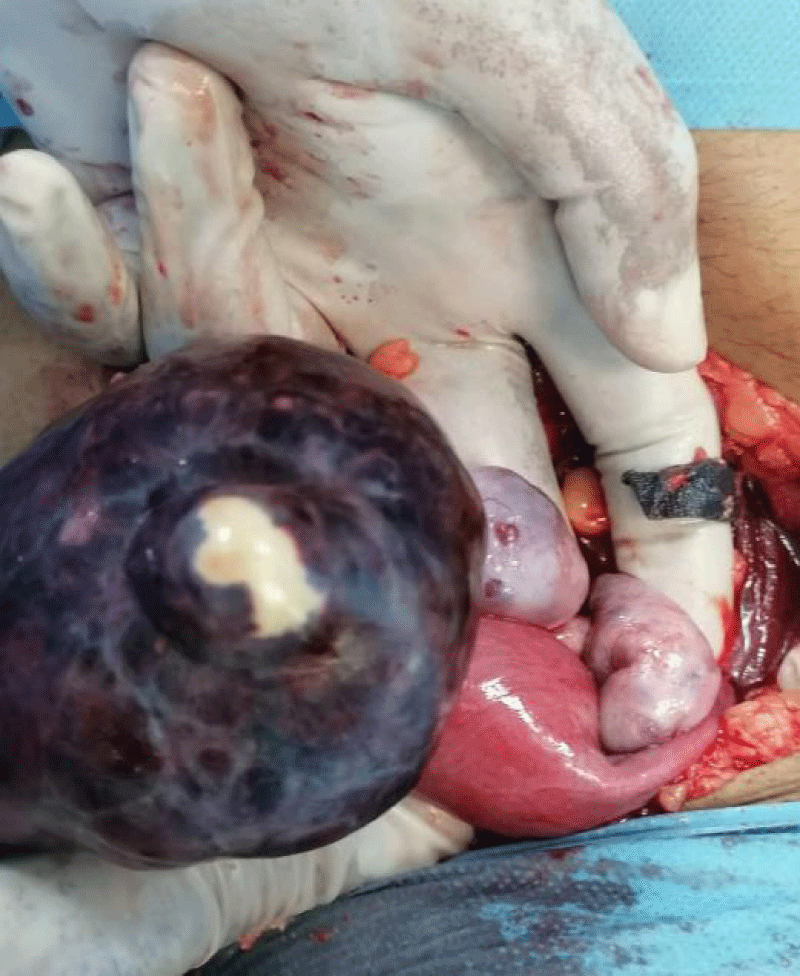
The patient was stabilized and an Ultrasound (USS) performed by the radiology department reported a twisted ovarian cyst. Patient went for laparotomy; intraoperative finding was large gangrenous pedunculated uterine fibroid and normal healthy ovaries (Pictures 1,2). The diagnosis confirmed by histopathology report.
Picture 1: Very twisted fibroid pedicle causing ischemic gangrene.
Picture 2: The gangrenous fibroid with healthy both ovaries.
There is special challenge for management of acute abdomen due to uterine fibroid. In order to overcome this problem clinicians need to use combination of clinical sense, radiological methods, and laboratory investigations.
Severe abdominal pain in fibroid is due to: degeneration, torsion or hemorrhage. Torsion is due to complete twisting of the pedicle leading to necrosis and gangrene presenting with severe pain, infection and peritonitis [3]. In general, ischemic pain due to torsion tends to be intermittent in nature, but at the end it become constant.
Ultrasonography remains the primary modality for evaluating uterine fibroids. In General, on sonography, fibroids typically appear as a hypoechoic or heterogeneous mass depending on the ratio of connective tissue to smooth muscle and this also affected by whether there is degeneration or not [2].
There are important technical points when doing ultrasound for pelvic mass; firstly, obtaining a panoramic view is essential and secondly the uterus and ovaries should be seen in clear manner to avoid diagnostic confusion between a fibroid and ovarian mass (which was missed in our case) specially if degenerative changes take place. It is important to remember that Doppler ultrasound typically demonstrates circumferential vascularity, but fibroids that are necrotic or have undergone torsion will show no flow [4].
Magnetic resonance imaging (MRI) offers better assessment in the case of inconclusive sonographic results, an MRI examination can be performed to determine the origin of the adnexal mass [2].
Ischemic gangrene related to uterine fibroid is rare.
Late diagnosis of ischemic gangrene in uterine fibroid can lead to increased morbidity and mortality.
Radiologists need to be aware of imaging findings suggestive of uterine fibroid torsion.
Declarations
Ethical consideration: Written informed consent was obtained from the patient for publication.
Data availability: All available information is included in the manuscript.
- Seung Chul Han, Man-Deuk Kim, Dae Chul Jung, Myungsu Lee, Mu Sook Lee, Sung Il Park, et al. Degeneration of Leiomyoma in Patients Referred for Uterine Fibroid Embolization: Incidence, Imaging Features and Clinical Characteristics. Yonsei Med J.2012;54(1): 215-219. https://doi.org/10.3349/ymj.2013.54.1.215
- Winarto H, Simatupang ONN, Calvin D, Siregar TP, Andrijono. Diagnostic Challenge: Distinguishing Uterine Fibroid with Cystic Degeneration vs. Ovarian Cystic Malignancy. A Case Report. J Radiol Case Rep. 2023;17(4):1-12. https://doi.org/10.3941/jrcr.v17i4.4583
- Ueda H, Togashi K, Konishi I, Kataoka ML, Koyama T, Fujiwara T, et al. Unusual appearances of uterine leiomyomas: MR imaging findings and their histopathologic backgrounds. Radiographics. 1999;19 Spec No:S131-45. https://doi.org/10.1148/radiographics.19.suppl_1.g99oc04s131
- Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health. 2014;6:95-114. https://doi.org/10.2147/ijwh.s51083