More Information
Submitted: 05 March 2020 | Approved: 30 March 2020 | Published: 31 March 2020
How to cite this article: Saletti A, Bernardoni A, Borgatti L, Carità G, Farneti M, et al. CT perfusion-guided endovascular treatment of symptomatic cerebral vasospasm in a patient with perimesencephalic non-aneurysmal subarachnoid hemorrhage. Arch Case Rep. 2020; 4: 020-021.
DOI: 10.29328/journal.acr.1001033
Copyright License: © 2020 Saletti A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
CT perfusion-guided endovascular treatment of symptomatic cerebral vasospasm in a patient with perimesencephalic non-aneurysmal subarachnoid hemorrhage
Andrea Saletti1*, Andrea Bernardoni1, Luca Borgatti1, Giuseppe Carità1, Marco Farneti2,3, Onofrio Marcello1 and Enrico Fainardi4
1Neuroradiology Unit, Department of Radiology, University Hospital of Ferrara, Italy
2Neurosurgery Unit, Department of Neurosciences and Rehabilitation, University Hospital of Ferrara, Italy
3Anesthesiology and Intensive Care Unit, Department of Critical Care, University Hospital of Ferrara, Italy
4Neuroradiology Unit, Department of Radiology, Careggi Hospital, Florence, Italy
*Address for Correspondence: Andrea Saletti, Operative Unit of Neuroradiology, Department of Radiology, University Hospital of Ferrara, Cona Hospital, Via Aldo Moro n.8, Italy, Tel: +39 3666236319; Email: a.saletti@ospfe.it
Symptomatic vasospasm represents an uncommon complication of perimesencephalic nonaneurysmal subarachnoid hemorrhage (SAH) which is a benign form of SAH without any recognizable source of bleeding accounting for about 15% of non-traumatic SAH [1,2].
Here, we describe the case of a 36-year-old previously healthy women who was admitted at our emergency department with a 4-days persistent severe headache characterized by an acute onset. At entry, no neurological deficits, including meningism, were found on examination.
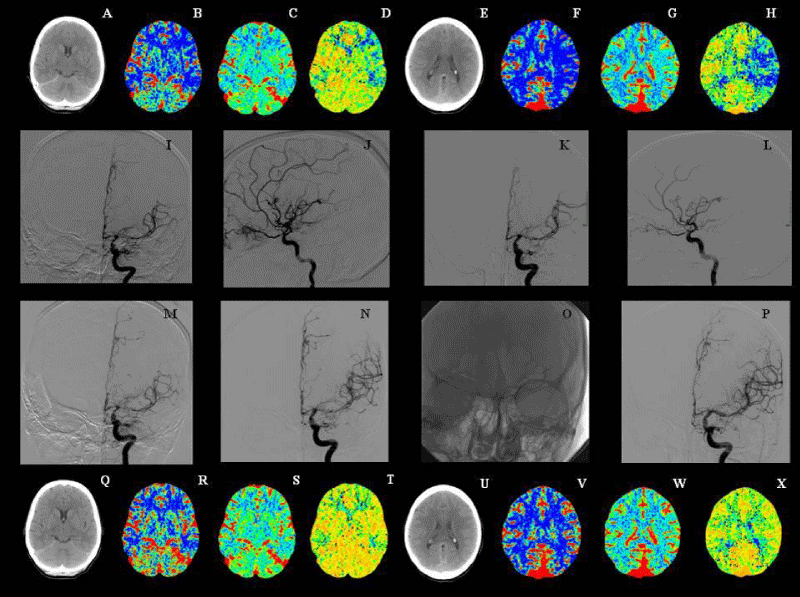
A CT scan showed a SAH located around the midbrain cisterns, whereas a CT angiography (CTA) and a 4-vessels cerebral digital subtraction angiography (DSA) were normal. In such a case we usually repeat a DSA after 14-20 days to confirm absence of any vascular malformation. A therapy with oral nimodipine was started. Eleven days after admission, she developed dysarthria and a slight right hemiparesis. A repeat CT scan detected a persistent small clot within the prepontine cistern, in absence of focal lesions or hydrocephalus. A CT perfusion (CTP) study performed on a 64-section CT scanner documented decreased cerebral blood flow (CBF) and prolonged mean transit time (MMT) associated with preserved cerebral blood volume (CBV) in the left middle cerebral artery (MCA) territory indicative of reversible ischemia (Figure 1 A-H). During the subsequent cerebral DSA, that confirm absence of any vascular malformation , a severe vasospasm in sovraclinoid segment of both internal carotid artery and in the M1 segment of left MCA was identified (Figure 1 I,J). According to the neurosuegeon we decided to start intra-arterial injection of 3 mg of nimodipine resulted in a mild improvement of angiographic picture (Figure 1 K,L) and a complete remission of clinical symptoms. Triple H therapy was then started . The day after a clinical worsening occurred since she experienced aphasia and a more pronounced right hemiparesis. A new cerebral DSA showed a recurrence of vasospasm (Figure 1 M) that was treated with the intra-arterial administration of 3 mg of nimodipine followed by balloon angioplasty performed by using an Hyperglide balloon 4 mm x 10 mm (EV3) due to the persistence of vessel narrowing (Figure 1 N,O). At the end of the procedure, a complete resolution of angiographic (Figure 1 P) and clinical abnormalities was observed. A second CTP examination carried out the day after indicated the normalization of CBF and MTT disturbances (Figure 1 Q-X). She was discharged two weeks later with a modified Rankin scale = 0 and a negative CT scan. This report confirms that perimesencephalic non-aneurysmal SAH can be complicated by a symptomatic cerebral vasospasm [1,2], for which endovascular treatment with nimodipine and balloon angioplasty is an effective procedure [3,4]. Our therapeutic approach was further justified by CTP findings demonstrating the presence of critically hypo perfused but potentially salvageable tissue at risk for infarction that, after treatment, was totally reperfused. CTP is a powerful tool for the diagnosis and management of vasospasm not only in aneurismal [5] but also in perimesencephalic non-aneurysmal SAH. In this form of SAH, as transcranial Doppler is not sensitive in determining the degree of vasospasm-related ischemia [6], visual inspection of CTP maps could be considered as the method of choice to guide the decision to treat due to its ability in establishing severity and temporal evolution of vasospasm [7,8].
Figure 1: Figure A-H: Standard CT scan and cerebral blood flow (CBF), cerebral blood volume (CBV) and mean transit time (MTT) CTP maps obtained 11 days after admission at the level of basal ganglia (A-D) and lateral ventricles (E-H) and showing reduced CBF, increased MTT and normal CBV in the left middle cerebral artery (MCA) territory, in absence of focal areas of hypoattenuation. Figure I-L: the following cerebral digital subtraction angiography (DSA) demonstrating a severe vasospasm in sovraclinoid segment of both internal carotid artery and in the M1 segment of left MCA (I-J) and its partial remission observed after the intra-arterial injection of nimodipine (K-L). Figure M-P: cerebral DSA performed 12 days after entry and illustrating the recrudescence of vasospasm (M), its initial improvement after nimodipine intra-arterial administration (N), balloon positioning in the left MCA (O) and the final resolution of arterial narrowing (P). Figure Q-X: Standard CT scan and CBF, CBV and MTT CTP maps acquired 13 days after admission at the level of basal ganglia (Q-T) and lateral ventricles (U-X) and documenting the complete restoring of cerebral perfusion in the left MCA territory.
- Schievink WI, Eelco FM, Wijdicks FM, Spetzler RF. Diffuse vasospasm after pretruncal nonaneurysmal subarachnoid hemorrhage. Am J Neuroradiol. 2000; 21: 521-523. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10730645
- Koçak A, Saraç K, Ateş SR, Çailý. Severe cerebral vasospasm caused by non-aneurysmal subarachnoid hemorrhage treatment with transluminal balloon angioplasty. Minim Invas Neurosurg. 2007; 50: 23-26. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17546539
- Biondi A, Ricciardi GK, Puybasset L, Abdennour L, Longo M, et al. Intra-arterial nimodipine for the treatment of symptomatic cerebral vasosopasm after aneurysmal subarachnoid hemorrhage: preliminary results. Am J Neuroradiol. 2004; 25: 1067-1076. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15205150
- Eskridge JM, McAuliffe W, Song JK, Deliganis AV, Newell DW, et al. Balloon angioplasty for the treatment of vasospasm: results of the first 50 cases. Neurosurgery. 1998; 42: 510-517. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9526985
- Greenberg ED, Gold R, Reichman M, John M, Ivanidze J, et al. Diagnostic accuracy of CT angiography and CT perfusion for cerebral vasospasm: a meta-analysis. Am J Neuroradiol. 2010; 31: 1853-1860. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20884748
- Ekelund A, Saveland H, Romner B, Brandt L. Is transcranial Doppler sonography useful in detecting late cerebral ischemia after aneurismal subarachnoid hemorrhage? Br J Neurorsurg. 1996; 10: 19-25. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8672254
- Dankbaar JW, de Rooij NK, Velthuis BK, Frijns CJ, Rinkel GJE, et al. Diagnosing delayed cerebral ischemia with different CT modalities in patients with subarachnoid hemorrhage with clinical deterioration. Stroke. 2009; 40: 3493-3498. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19762703
- Dankbaar JW, de Rooij NK, Smit EJ, Velthuis BK, Frijns CJ, et al. Changes in cerebral perfusion around the time of delayed cerebral ischemia in subarachnoid hemorrhage patients. Cerebrovasc Dis. 2011; 32: 133-140. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21778710