More Information
Submitted: January 10, 2023 | Approved: January 23, 2023 | Published: January 24, 2023
How to cite this article: Gabsi S, Aziz A, Hajri M, Hadrich Z, Omrani S, et al. Primary follicular lymphoma arising from the ascendant colon: A case report. Arch Case Rep. 2023; 7: 003-005.
DOI: 10.29328/journal.acr.1001065
Copyright License: © 2023 Gabsi S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Primary follicular lymphoma arising from the ascendant colon: A case report
Sofiene Gabsi, Atallah Aziz, Mohamed Hajri, Zied Hadrich* , Sahir Omrani, Rached Bayar and Hafedh Mestiri
, Sahir Omrani, Rached Bayar and Hafedh Mestiri
Department of General Surgery, Mongi Slim University Hospital, Faculty of Medicine of Tunis, University of Tunis El Manar, Tunisia
*Address for Correspondence: Zied Hadrich, Department of General Surgery, Mongi Slim University Hospital, Faculty of Medicine of Tunis, University of Tunis El Manar, Tunisia, Email: hadrich1988@gmail.com
Lymphomas are common hematological malignancies with an increasing incidence in recent years. The main site of extranodal non-Hodgkin’s lymphoma is the gastrointestinal tract, representing 40% of cases. The most common site of gastrointestinal lymphoma is the stomach, followed by the small intestine, accounting for 25% - 50% and 20% - 30%, respectively [1,2]. Primary colorectal lymphoma is a rare disease, accounting for 0.2% to 1% of all colorectal malignancies [1]. Males are more commonly affected with a peak incidence in the sixth and seventh decades of life [3]. Non-Hodgkin’s lymphoma is the most commonly described subtype of colonic lymphoma [1].
We report a case of primary follicular lymphoma of the right colon complicated by subocclusive syndrome treated with surgery and then chemotherapy.
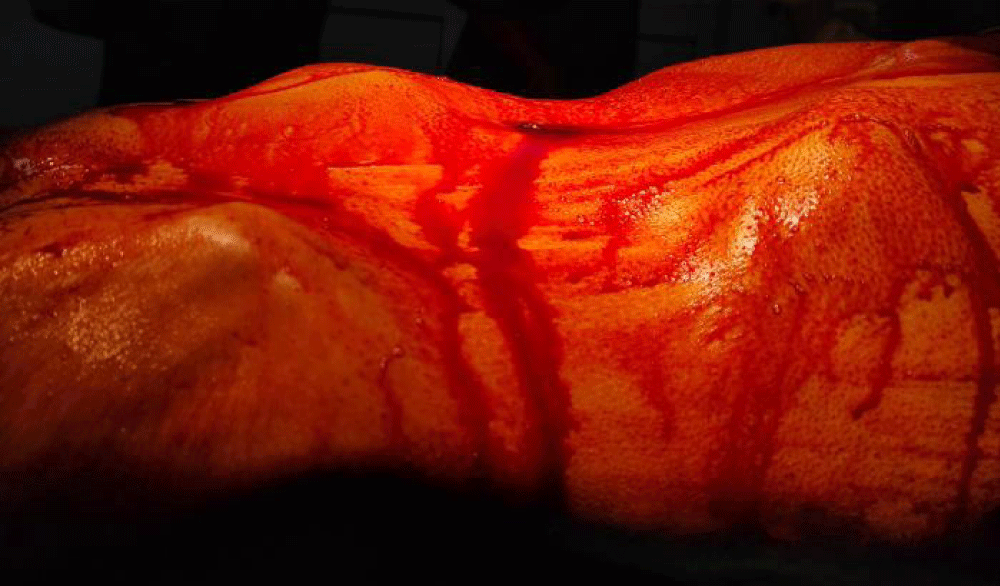
A 63-year-old male presented with a history of abdominal pain, bloating, vomiting, and chronic constipation, together with an estimated weight loss of 20 kg over 2 months. Physical examination revealed a non-tender, firm mass in the right lower quadrant with respect to the superficial plans (Figure 1). There was no hepatomegaly or splenomegaly and no palpable associated lymph nodes. A complete colonoscopy revealed a large vegetative lesion of the ascending colon with partial luminal obliteration. Biopsy findings were inconclusive. Tumor marker concentrations were within normal limits.
Figure 1: Abdominal examination disclosed a renitent firm mass in the lower right cadrant.
A computed tomography scan (Figure 2) showed a 100x56x95 mm mass of the right colon with evidence of invasion of the Bauhin valve. No metastatic lesions were found. The patient underwent surgery and a right hemicolectomy with manual ileocolic anastomosis was performed. The postoperative period was uneventful, the patient was discharged 6 days after surgery.
Figure 2: Axial Contrast-enhanced computed tomography scan demonstrated a mass of 100 mm x 56 mm x 95 mm of the right colon (yellow asterisk).
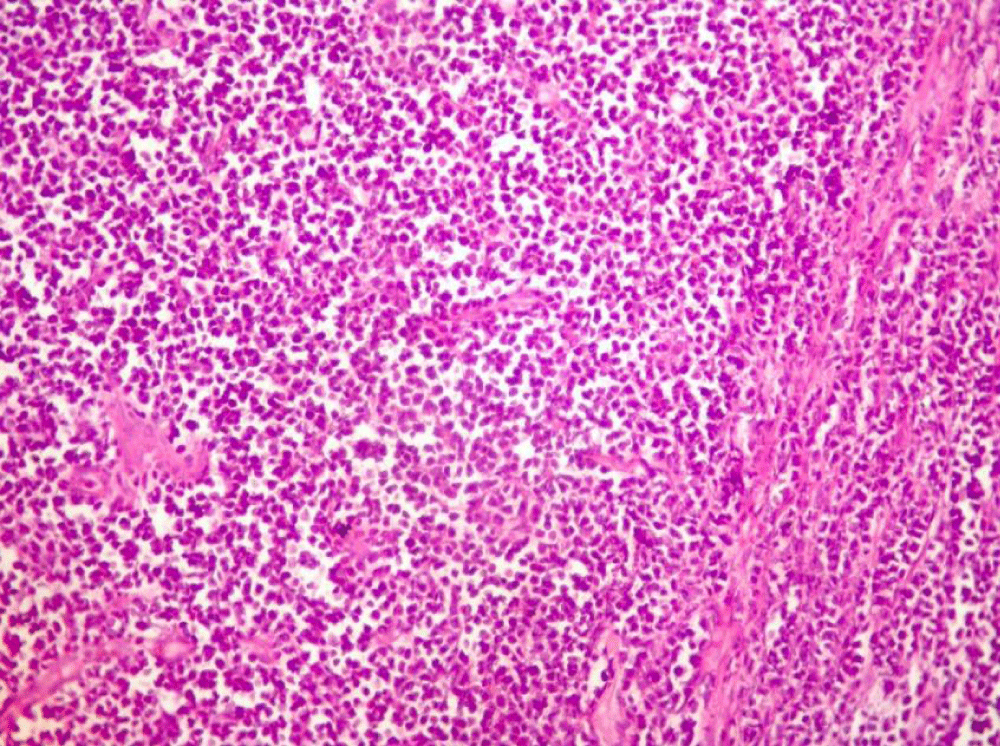
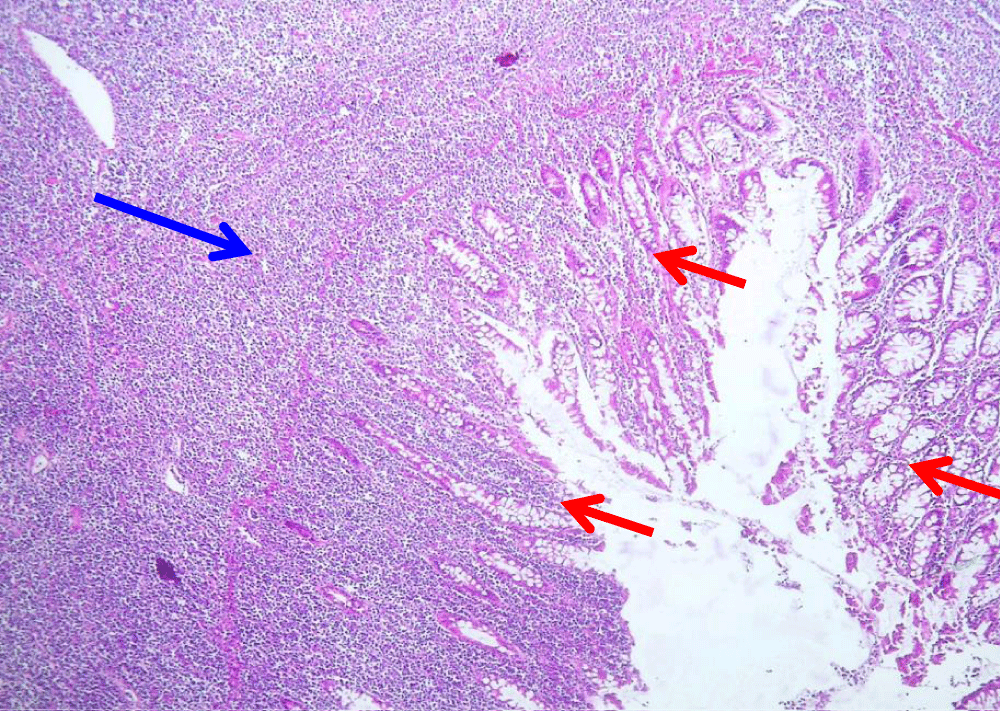
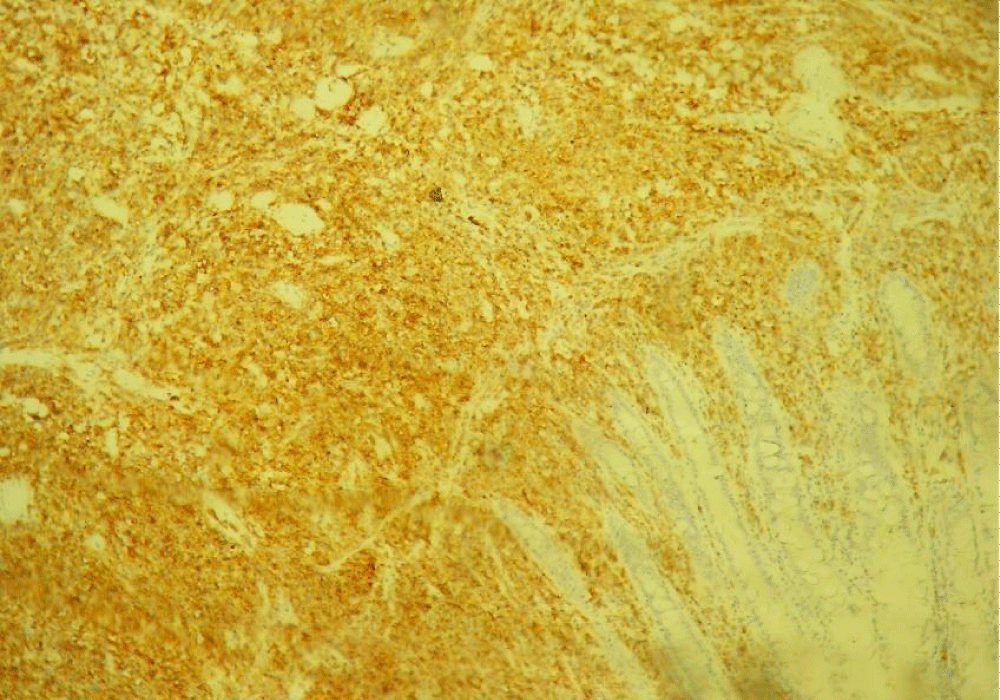
The pathological result (Figures 3-6) of the resected colon showed a proliferative lymphoid tumor without nodular aspects. An immunohistochemical study showed positivity for CD20, BCL2 and CD10 antibodies. 3 lymph nodes were metastatic out of a total of 38 lymph nodes analyzed. A few weeks after the operation, he was referred for postoperative chemotherapy.
Figure 3: On gross examination (after formalin fixation): Withish cecal tumor with a “fish flesh” aspect measuring 12 cm x 10 cm x 11 cm.
Figure 4: Histological findings of the colonic tumor showing small tumor cells with a mottled chromatin nucleus thats is sometimes nucleolated and mitotic (Hematoxylin and eosin, magnification X 250).
Figure 5: Dense and diffuse lymphomatous proliferation invading the entire thickness of the colonic wall (Blue Arrow). Red arrows show residual colonic mucosa (Hematoxylin and eosin, magnification X 250).
Figure 6: Immunohistochemical study showing positive immunostaining of the tumor cells with the CD20 antibody.
Primary colonic lymphoma (PCL) is a very rare neoplasm accounting for less than 1% of all colonic malignancies. Usually arising from the B-cell lineage, this entity has a variety of subtypes [3].
The most frequent site of this neoplasm is the cecum, most likely due to the excess lymphatic tissue in this region [1].
In the absence of specific complaints, the diagnosis is often difficult to make. Unfortunately, in some cases, the diagnosis can only be made by surgery. In addition, there is a delay in the diagnosis in 33% to 65% of patients, making the intervention urgent because of the occlusive complications that it can cause [4,5], as in our case.
In more than half of the cases, a large mass of more than 5 cm is palpable on physical examination [6]. Colonoscopy is a valuable diagnostic tool for colonic lymphoma in the absence of an emergency context. However, it is not always possible due to technical malfunction (inadequate biopsy) and the need to perform immunohistochemical staining. In these cases, as in ours, surgery will provide a definitive diagnosis [4].
The main treatment for uncomplicated colorectal lymphoma is a combination of surgery and postoperative chemotherapy. Multiple studies showed that early-stage disease should be treated with surgery associated with multidrug postoperative chemotherapy as it has significant improvement in short-term mortality [1,3]. Advanced and uncomplicated PCL are treated with only chemotherapy [2], which may improve the progression-free and overall survival. However, due to the effectiveness of newer targeted drugs, CD20-positive B-cell lymphomas can be treated with a combination of polychemotherapy and immunotherapy, with long-lasting efficacy.
However, most patients undergo emergent surgery due to bowel obstruction or colonic perforation as a result of a delayed diagnosis [4]. Cai, et al. reported in their series of 43 patients that 56% of them required emergency surgery [5]. Our patient presented continuous abdominal pain and subocclusive syndrome, so we opted for surgical treatment followed by adjuvant chemotherapy.
The aim of our study is to raise the awareness of the surgeon and the clinician about this uncommon disease, whose prognosis will depend on the precocity of the diagnosis.
We report the case of a 63-year-old man who underwent surgery for a right colon tumor which turned out to be a primary lymphoma. It is an exceptional entity, diagnosed late and confirmed by surgery. The modalities of its management are unclear and not standardized due to its rarity, but a multidisciplinary approach is necessary for better outcomes in this malignancy associated with poor prognosis.
- Meir E, Handler C, Kaplan U, Kopelman D, Hatoum OA. Primary small cell type of non-Hodgkin lymphoma of the colon: a case report. J Med Case Rep. 2020 Sep 19;14(1):157. doi: 10.1186/s13256-020-02500-y. PMID: 32948246; PMCID: PMC7501666.
- Pascual M, Sánchez-González B, García M, Pera M, Grande L. Primary lymphoma of the colon. Rev Esp Enferm Dig. 2013 Feb;105(2):74-8. doi: 10.4321/s1130-01082013000200003. PMID: 23659505.
- Maguire LH, Geiger TM, Hardiman KM, Regenbogen SE, Hopkins MB, Muldoon RL, Ford MM, Hawkins AT. Surgical management of primary colonic lymphoma: Big data for a rare problem. J Surg Oncol. 2019 Sep;120(3):431-437. doi: 10.1002/jso.25582. Epub 2019 Jun 11. PMID: 31187517.
- Won RP, Lin MYC, Williams JL, Petrie BA. Primary Colonic Lymphoma. J Gastrointest Surg. 2018 Feb;22(2):361-362. doi: 10.1007/s11605-017-3472-4. Epub 2017 Nov 29. PMID: 29188491.
- Cai S, Cannizzo F Jr, Bullard Dunn KM, Gibbs JF, Czuczman M, Rajput A. The role of surgical intervention in non-Hodgkin's lymphoma of the colon and rectum. Am J Surg. 2007 Mar;193(3):409-12; discussion 412. doi: 10.1016/j.amjsurg.2006.12.007. PMID: 17320545.
- Stanojević GZ, Stojanović MP, Stojanović MM, Krivokapić Z, Jovanović MM, Katić VV, Jeremić MM, Branković BR. Non-Hodgkin's lymphomas of the large bowel-clinical characteristics, prognostic factors and survival. Acta Chir Iugosl. 2008;55(3):109-14. doi: 10.2298/aci0803109s. PMID: 19069702.